Eur J Heart Fail:需要机械通气且伴有急性呼吸窘迫综合征的COVID-19患者血流动力学特征
2020-11-26 MedSci原创 MedSci原创
需要机械通气的COVID-19患者血流动力学特征是心肺功能改变。肺血管阻力低、缺氧性血管收缩减弱与高心输出量和毛细血管后肺动脉高压相关,并最终可能导致肺硬化,并在肺脏与心脏之间形成恶性循环。
由于2019冠状病毒病(COVID-19)导致的间质性肺炎通常并发严重的呼吸衰竭。除了降低肺顺应性和通气/灌注不匹配外,还可能有低氧性肺血管收缩,这可能解释了COVID-19患者心肺综合征的特殊病理生理学机制。但是,到目前为止,尚无关于COVID-19患者有创血流动力学特征的报道。
近日,心血管领域权威杂志European Journal of Heart Failure上发表了一篇研究文章,21例机械通气的COVID-19患者接受了右心导管检查。研究人员将他们的数据与年龄、性别和体重指数匹配的非机械通气配对照者数据进行了比较,并与来自系统性文献综述的1937名“典型”急性呼吸窘迫综合征(ARDS)患者的汇总数据进行了比较。
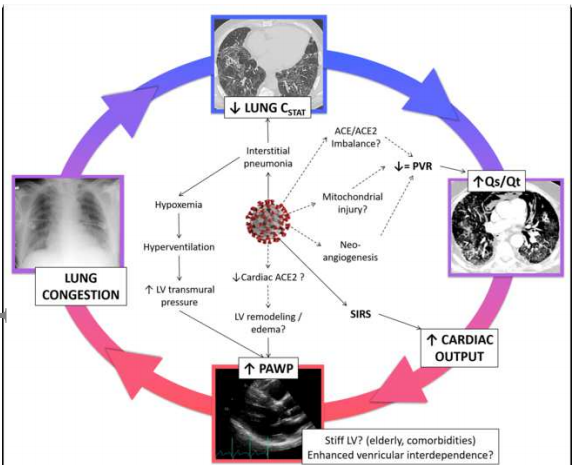
COVID-19患者的心脏指数高于对照者(3.8 [2.7-4.5] vs 2.4 [2.1-2.8] L/min/m2,p<0.001),但略低于ARDS(p=0.024)。肺内分流和肺顺应性与COVID-19呈负相关(r=-0.57,p=0.011),而与ARDS并无差异。尽管,COVID-19患者的肺血管阻力仍正常,但与对照组相似(1.6 [1.1-2.5] vs 1.6 [0.9-2.0] WU,p=0.343),并且低于ARDS患者中的报告数据(p<0.01)。76%的COVID-19患者和19%的对照者均存在肺动脉高压(p<0.001),并且毛细血管后肺动脉高压常见。COVID-19患者肺动脉楔压高于ARDS患者,并且与肺顺应性呈负相关(r=-0.46,p=0.038)。
由此可见,需要机械通气的COVID-19患者血流动力学特征是心肺功能改变。肺血管阻力低、缺氧性血管收缩减弱与高心输出量和毛细血管后肺动脉高压相关,并最终可能导致肺硬化,并在肺脏与心脏之间形成恶性循环。
原始出处:
Sergio Caravita.et al.Hemodynamic characteristics of COVID‐19 patients with acute respiratory distress syndrome requiring mechanical ventilation. An invasive assessment using right heart catheterization.European journal of heart failure.2019.https://onlinelibrary.wiley.com/toc/18790844/0/ja
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#血流动力#
41
#COVID-19患者#
56
#ART#
52
#血流动力学#
54
#综合征#
44
#HEART#
60
#呼吸窘迫#
71
肺血管阻力低、缺氧性血管收缩减弱与高心输出量和毛细血管后肺动脉高压相关,并最终可能导致肺硬化,并在肺脏与心脏之间形成恶性循环。
115