Ther Adv Med Oncol:国内多中心头对头III期研究发现转移性结直肠癌患者二线FOLFIRI方案并不优于单药伊立替康治疗,反而毒性增加
2022-01-15 yd2015 MedSci原创
该研究是首个头对头研究并发现,对于一线XELOX/FOLFOX方案治疗失败的mCRC患者,二线单药伊立替康获得跟FOLFIRI方案治疗类似的PFS、OS和ORR,且毒性更少。
FOLFIRI[伊立替康、亚叶酸(CF)和氟尿嘧啶]被认为是一线XELOX/FOLFOX方案失败的转移性结直肠癌(mCRC)患者的标准二线化疗方案。然而,目前还不清楚氟尿嘧啶在这种情况下是否仍然必要。因此,国内学者开展了头对头的III期研究,旨在评估FOLFIRI作为mCRC患者二线治疗方案是否优于单药伊立替康。相关结果发表在Therapeutic Advances in Medical Oncology杂志上。

该研究(NCT02935764)是在中国五家医院进行的,随机,多中心,开放标签,III期临床研究。从2016年11月4日至2020年1月17日,筛选和入组≧18岁经组织学证实不能切除以及一线XELOX/FOLFOX方案失败的mCRC患者。患者随机接受FOLFIRI或伊立替康治疗。主要终点为无进展生存期(PFS)。次要终点包括总生存期(OS)、客观缓解率(ORR)和毒性。
共有172名mCRC患者随机接受FOLFIRI (n = 88)或伊立替康(IRI,n = 84)治疗。FOLFIRI组88例患者有78例(88.6%)因为疾病进展[58例(65.9%)],AE 9例(10.2%),病人拒绝7例(8.0%),和改变其他治疗[4](4.5%)而中断治疗;IRI组84例患者有74例(89.2%)因为疾病进展[50 (59.5%)],AE[4](4.8%),病人拒绝13例(15.9%),改用其他治疗[6例(7.1%)]和CR[1例(1.2%)]而中断治疗。
FOLFIRI组的中位PFS为104天(3.5个月;95% CI = 85-123天),IRI组为112天(3.7个月;95% CI = 92-132天),两组中位PFS没有统计学差异(HR = 1.084, 95% CI = 0.7911-1.485;p = 0.6094)。两组的中位OS分别为420天(14个月; 95% CI = 349–491天)和408天(13.6个月; 95% CI = 325–491天) ,同样也没有统计学差异(HR = 0.9466,95% CI = 0.6553–1.368; p = 0.7689)。
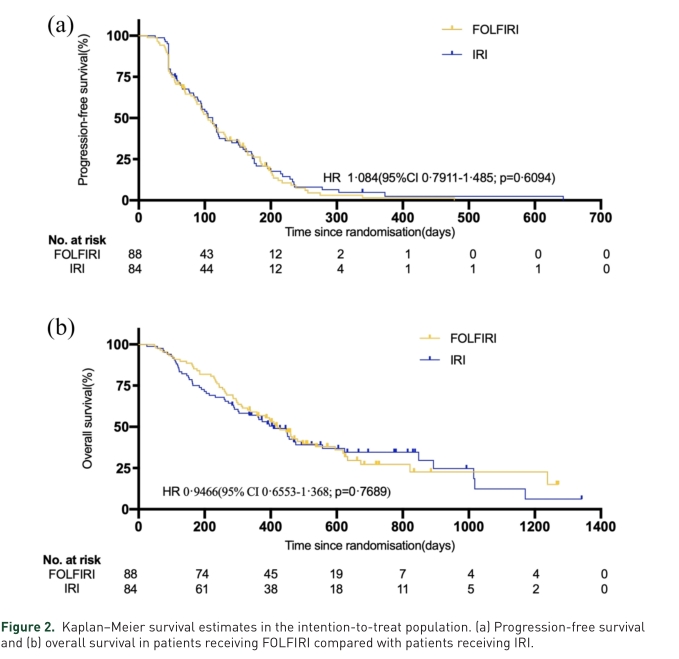
两组的PFS和OS差异
两组的ORR分别为6.8%和7.1%,没有统计学差异(p=0.933)。
FOLFIRI组的下列不良事件(AEs)发生率显著高于伊立替康组:任何级别的AEs包括白细胞减少(73.9% vs 55.4%)、中性粒细胞减少(72.7% vs 56.6%)、血小板减少(31.8% vs 18.1%)、黄疸(18.2% vs 7.2%)、粘膜炎(40.9% vs 14.5%)、呕吐(37.5% vs 21.7%)、发烧(19.3% vs 7.2%)和3 - 4级中性粒细胞减少(47.7% vs 21.7%)。
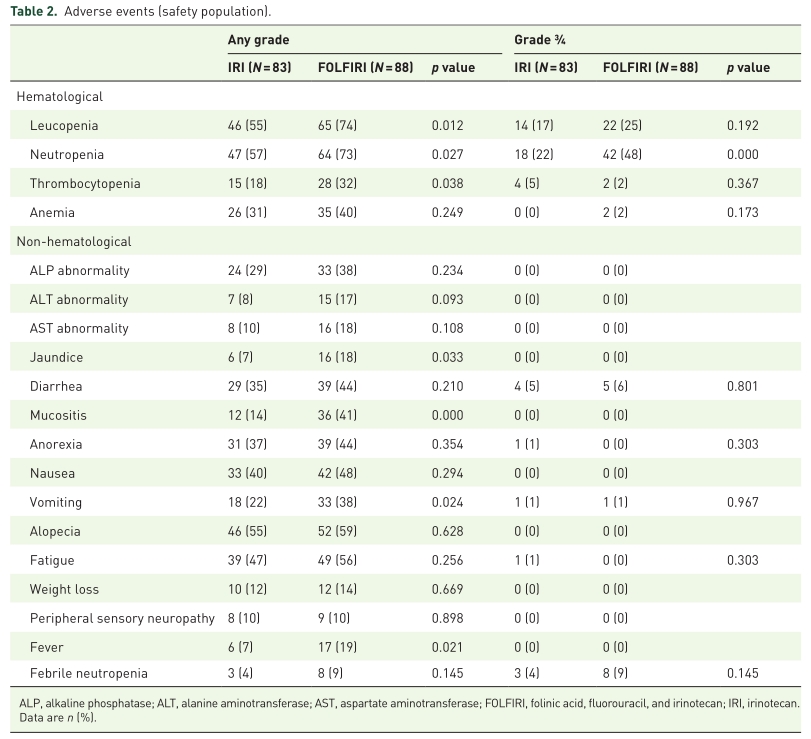
两组的不良事件
同样,亚组探索性分析也表明在所有亚组中,FOLFIRI治疗并不优于单药伊立替康。

亚组分析
综上,该研究是首个头对头研究并发现,对于一线XELOX/FOLFOX方案治疗失败的mCRC患者,二线单药伊立替康获得跟FOLFIRI方案治疗类似的PFS、OS和ORR,且毒性更少。
原始出处:
Xiaowei Zhang, Ran Duan, Yusheng Wang, et al. FOLFIRI (folinic acid, fluorouracil, and irinotecan) increases not efficacy but toxicity compared with single-agent irinotecan as a second-line treatment in metastatic colorectal cancer patients: a randomized clinical trial. Ther Adv Med Oncol.2022, Vol. 14: 1-12. DOI: 10.1177/17588359211068737.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#III期研究#
85
#III#
62
#多中心#
85
#研究发现#
100
#FOLFIRI方案#
74
#Oncol#
56
#头对头#
70
#转移性#
76
#结直肠#
84
#FOLFIRI#
97