硬脊膜外脓肿手术
2016-03-14 MedSci www.windrug.com
硬脊膜外脓肿手术 椎管内硬脊膜外间隙的化脓性炎症在椎管内化脓性炎症中比较常见。皮肤疖疮为最主要原发感染灶,致病菌绝大多数是金黄色葡萄球菌,血行播散最为常见。多发生于胸椎上段背面,它引起脊髓损害症状,多半急剧而严重;如手术治疗及时,大多可治愈,哪延误诊断将造成严重残废,甚至死亡。 [适应证] 硬脊膜外脓肿临床诊断成立,或腰椎穿刺、椎旁穿刺抽出脓液,或脊髓造影证实有脊髓压迫者均应手术治疗。病情发
硬脊膜外脓肿手术
椎管内硬脊膜外间隙的化脓性炎症在椎管内化脓性炎症中比较常见。皮肤疖疮为最主要原发感染灶,致病菌绝大多数是金黄色葡萄球菌,血行播散最为常见。多发生于胸椎上段背面,它引起脊髓损害症状,多半急剧而严重;如手术治疗及时,大多可治愈,哪延误诊断将造成严重残废,甚至死亡。
[适应证]
硬脊膜外脓肿临床诊断成立,或腰椎穿刺、椎旁穿刺抽出脓液,或脊髓造影证实有脊髓压迫者均应手术治疗。病情发展急剧而严重者应视为神经外科急症。
[术前准备]
同椎管-脊髓探查术。
[麻醉]
全麻或局麻。
[手术步骤]
1.体位 侧卧位或俯卧位。
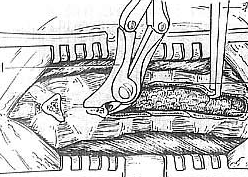
2.以病灶为中心作后背正中切口。如脓肿已穿破椎管,形成椎旁脓肿,则在显露棘突及椎板过程中即可见到脓液,否则,先在病灶中心咬除1~2个椎板即可见到硬脊膜外脓肿,然后再根据病变范围向上下两端扩大,一边显露,一边清除脓液,要使硬脊膜显露区上下均出现搏动。病变部位的椎板和椎体如有化脓性骨髓炎,骨质松软易碎,在从椎板上剥离肌肉时应小心,不可用力过猛,以防损伤脊髓。椎板切除不要损伤关节面,硬脊膜外肉芽组织应予轻轻刮除,注意勿损伤硬脊膜。尽量不要将骨蜡或明胶海绵遗留在伤口内,以免引起异物反应。不可切开硬脊膜,以免感染向硬脊膜下腔扩散[图1-1~7]。
 |
| 1-1 切口 |
 |
| 1-2 显露棘上棘带 |
 |
| 1-3 剥离骶棘肌 |
 |
| 1-4 干纱布填塞止血 |
 |
| 1-5 切除棘间韧带 |
 |
| 1-6 剪除棘突 |
 |
| 1-7 切除椎板 |
| 图1 椎管-脊髓探查术 |
3.在炎症未扩散到肌层或手术中发现主要为肉芽组织、创口污染不严重的病例,可缝合全部切口。一般感染较重者,仍以放置引流管较为安全。引流管于24~48小时后拔除。感染严重,脓液广泛扩散至肌层,估计引流无效的病例,可于伤口内填塞纱布引流,以后逐日拔除,残留伤口待肉芽组织生长或二期缝合。
[术中注意事项]
手术中如果发现脓液自硬脊膜下溢出,则可沿该处穿刺抽脓,或扩大硬脊膜溢脓孔,吸出脓液,脓腔冲洗,但不可将已与脊髓粘连的蛛网膜强行剥离,以免扩散炎症或损伤脊髓。
[术后处理]
同椎管-脊髓探查术。伤口脓液应作细菌培养及抗生素敏感试验,全身选用适当抗生素。伤口脓液引流较多者,可在引流管拔出前向伤口内注入抗生素溶液。在引流脓液的同时,必须有效地控制全身感染。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言







不错的文章
107
图片漂亮
128
#硬脊膜#
50
#脓肿#
66