Stroke:症状性颈动脉狭窄患者血小板粘附抑制剂Revacept的疗效
2022-06-15 MedSci原创 MedSci原创
症状性颈内动脉(ICA)狭窄患者是缺血性卒中复发的高危人群,120 mg Revacept治疗可降低症状性ICA狭窄患者的联合安全性和有效性终点。
症状性颈内动脉(ICA)狭窄患者是缺血性卒中复发的高危人群,需要早期介入治疗和抗血小板治疗。出血发生率增加可能会抵消围手术期强化血小板抑制的疗效。
近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员的目的是探究糖蛋白VI竞争性拮抗剂-Revacept来辅助标准抗血小板治疗是否能减少症状性ICA狭窄患者缺血性病变的发生几率。

在这项国际、多中心(16个地区)、随机(1:1:1)、双盲、安慰剂对照的平行组研究纳入了有症状的ICA狭窄患者。在符合威廉亚洲博彩公司 的抗血小板治疗之外,单次输注安慰剂、40mg或120mg Revacept,以评估疗效终点:治疗开始后扩散加权磁共振成像上新的缺血性病变的数量。该研究的主要临床结局为联合安全性和有效性终点,包括随访期间任何卒中或死亡、短暂性脑缺血发作、心肌梗死、冠状动脉介入和出血并发症。
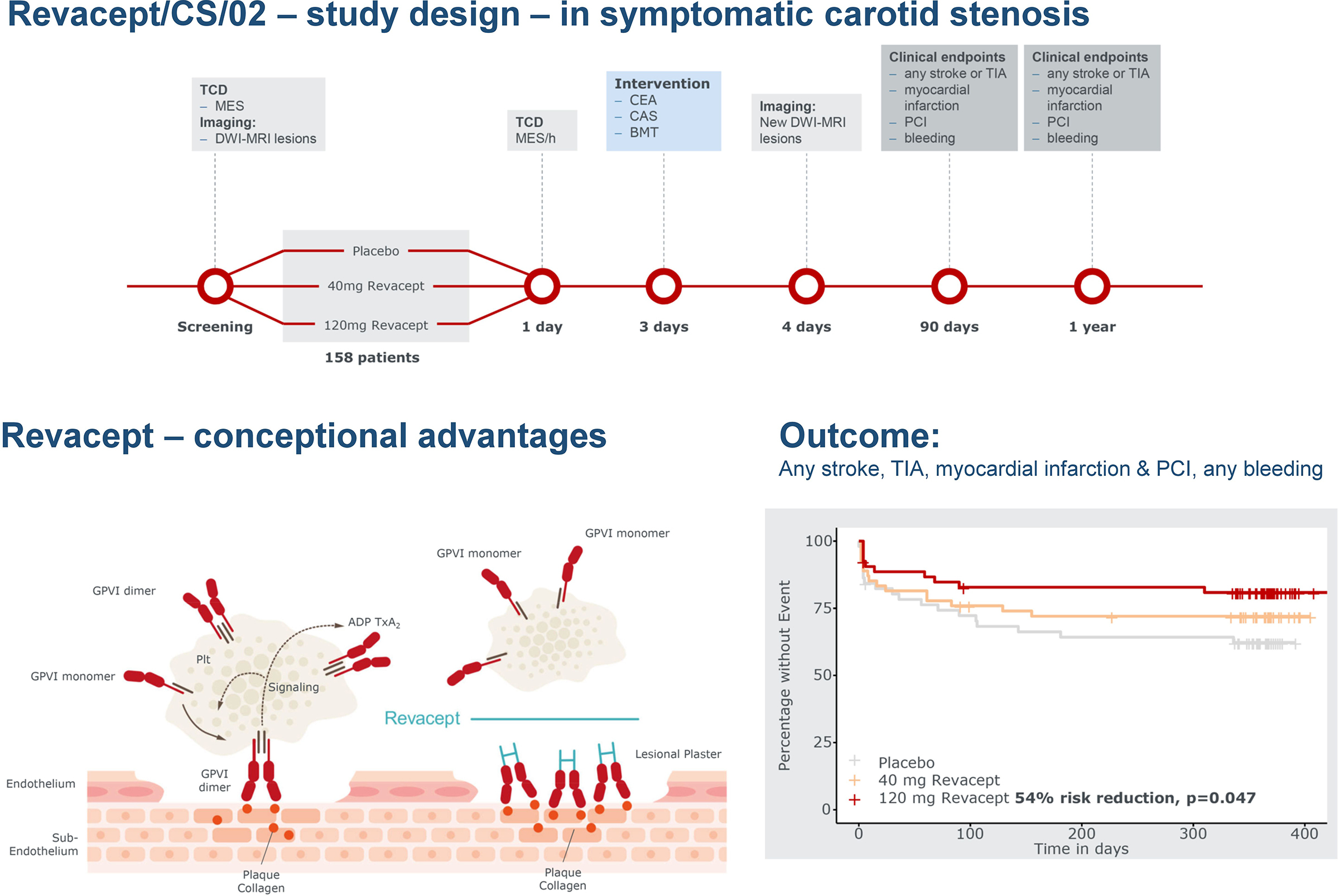
在160名随机患者中,158名患者(68±10.1年,24%为女性)接受了研究药物治疗(51名患者为安慰剂,54名患者为40mg Revacept,53名患者为120mg Revacept),随访11.2±2.3个月,在安慰剂/40mg/120mg Revacept治疗组中每名患者分别有1.16(95%CI为0.88-1.53)/1.05(95%CI为0.78-1.42;P=0.629)/0.63(95%CI为0.43-0.93)处检测到了新发弥散加权磁共振成像病变,且没有统计学上的差异。在研究期间,相比于安慰剂组,在服用120 mg Revacept的患者中观察到了联合安全性和有效性终点降低(HR为0.46[95%CI为0.21-0.99];P=0.047),而在40mg Revacept组中则不然(HR为0.72[95%CI为0.37-1.42];P=0.343)。
由此可见,120 mg Revacept治疗可降低症状性ICA狭窄患者的联合安全性和有效性终点。
原始出处:
Timo Uphaus.et al.Revacept, an Inhibitor of Platelet Adhesion in Symptomatic Carotid Stenosis: A Multicenter Randomized Phase II Trial.stroke.2022.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.037006
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#ACEP#
58
#颈动脉#
66
#症状性颈动脉狭窄#
64
#ACE#
96
#抑制剂#
56
#ACEP#
76
#动脉狭窄#
69