药物性肝损伤如何处理,一文总结
2021-08-05 zyyzjy MedSci原创
药物性肝损伤(DILI)占非病毒性肝病的20%-50%,占急性肝损伤住院患者的20%,是临床上最常见的药物不良反应之一!
药物性肝损伤(drug‑induced liver injury,DILI)的发生率为1.4% -8.1%,占非病毒性肝病的20%-50%,占急性肝损伤住院患者的20%,是临床上最常见的药物不良反应之一,若治疗不及时,可进展为肝衰竭,危及生命,所以也是最严重的药物不良反应之一,因此临床上应加以重视。
1.哪些药物可引起肝损伤?
1)目前明确引起DILI的药物超过1000种,包括非甾体类抗炎药、抗感染药物(含抗结核药物)、抗肿瘤药、中枢神经系统用药、心血管系统用药、代谢性疾病用药、激素类药物、生物制剂、传统中药、天然药、保健品、膳食补充剂等,其中中药、膳食补充剂及抗结核药是我国DILI的主要原因,对乙酰氨基酚是引起急性肝衰竭最主要的原因。
2.DILI分类
1)根据发生的可预见性分类:
导致DILI的药物分为可预测性和不可预测性两类;
①可预测性药物是指一旦过量或超长疗程使用该药物,大多数人出现肝损伤,呈剂量、疗程依赖性,代表性药物有对乙酰氨基酚、胺碘酮、环磷酰胺、环孢素、甲氨蝶呤等;
②不可预测性药物是指肝损伤程度与药物剂量和疗程无关,常发生在一些过敏或代谢特异体质的患者,由机体免疫介导;
大多数药物引起的DILI是不可预测的。此外值得注意的是不同药物可导致相同类型肝损伤,同一种药物也可导致不同类型的肝损伤。
2)按病程分:
①急性DILI:
DILI发生6个月内,肝功能恢复正常,无明显影像学和组织学肝功能损伤证据。其占DILI的90%以上,多发生在用药后的第5-90天。
②慢性DILI:
DILI发生6个月后,血清 ALT、AST、ALP 及TBil仍持续异常,或存在门静脉高压或慢性肝损伤的影像学和组织学证据。
3)按受损靶细胞分:
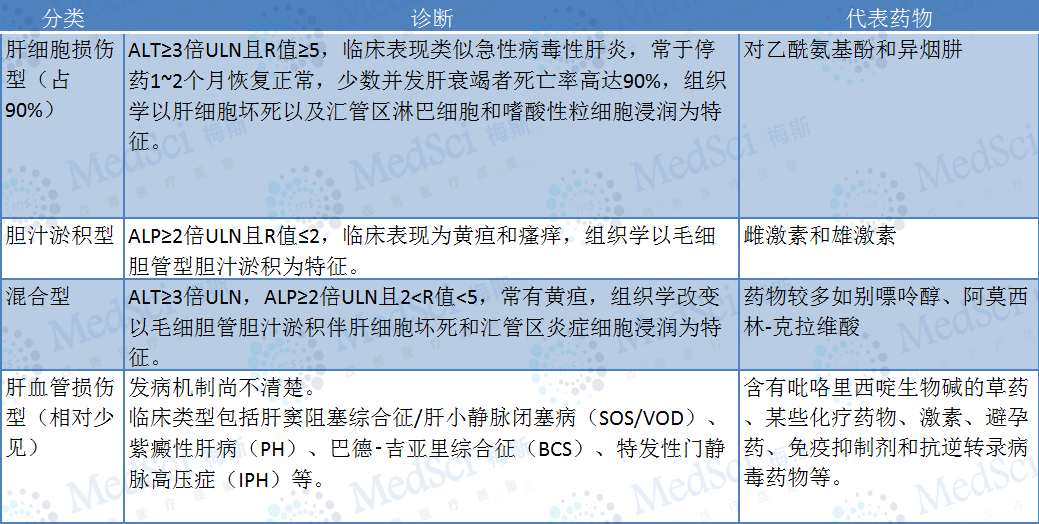
注:R值=血清(ALT实测值/ALT的正常值上限ULN)/(ALP实测值/ALP的ULN)
3.DILI有哪些危险因素?
①宿主因素:分为遗传因素和非遗传因素,包括高龄、女性、妊娠、饮酒、联合使用药物、合并慢性肝病、合并艾滋病等。
②药物因素:包括药物的化学性质、剂量、疗程、药物相互作用、中药材种植和炮制等过程中的污染等常可影响DILI的潜伏期、临床类型、病程和结局。
③环境因素:过量饮酒可能增加度洛西汀、对乙酰氨基酚、甲氨蝶呤及异烟肼等引起DILI的风险。吸烟对DILI易感性的影响尚不清楚。
4. DILI的诊断
①有药物暴露史;
②排除其他原因或疾病所致的肝功能损伤;
③可能有危险因素和药物说明书含有肝毒性信息;
④肝脏损伤在相应的潜伏期,通常1-4周;
⑤停药后,肝功能指标有所改善;
⑥偶尔再次给药,迅速激发肝损伤。
其中①②是诊断DILI的必要条件,③-⑥是非必要条件。
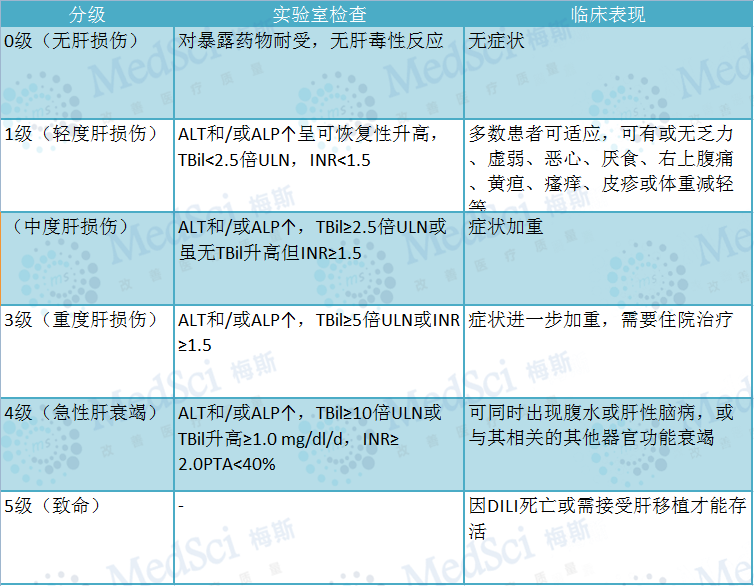
5. DILI严重程度分级
6. DILI的治疗
1)基本治疗原则:
①及时停用可疑肝损伤药物,尽量避免再次使用可疑或同类药物;
②应充分权衡停药引起原发病进展和继续用药导致肝损伤加重的风险;
③根据DILI的临床类型选用适当的药物治疗;
④重症患者必要时可考虑紧急肝移植。
2)停药
出现下列情况之一应考虑停用肝损伤药物:
①血清ALT或AST>8倍ULN;
②ALT或AST>5倍ULN,持续2周;
③ALT或AST>3倍ULN,且TBil>2倍ULN或INR>1.5;
④ALT或AST>3倍ULN,伴逐渐加重的疲劳、恶心、呕吐、右上腹疼痛或压痛、发热、皮疹和/或嗜酸粒细胞增多(>5%)。
多数患者在停用肝损伤药物后可完全恢复。
3)保肝药物:
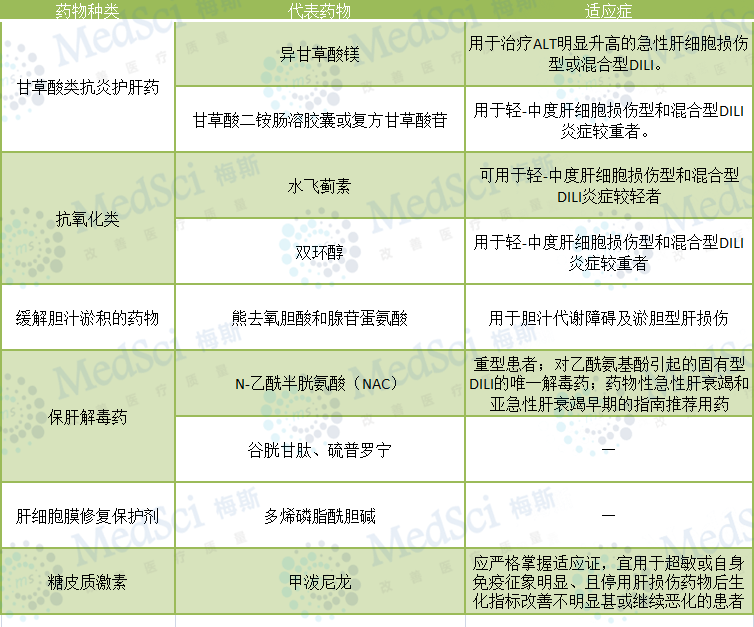
4)保肝药物选择原则:
①简化用药。最好选择1种具有多重作用机制的药物,必要时可考虑不同作用机制的药物联用。
②选择疗效确切的药物。
③大多数药物以口服途径用药,肝功能衰竭时静脉给药为主,也可静脉滴注后改为口服的序贯治疗。
④注重药物安全性。用药期间应定期观察患者的症状、体征和肝功能变化,必要时及时调整用药方案。
5)急性肝衰竭治疗:
重症DILI一旦患者发生急性肝衰竭且经内科治疗不能逆转或预后凶险,应及时行人工肝支持或肝移植治疗。
7.预后
急性DILI患者大多预后良好。
慢性DILI的预后总体上好于组织学类型相似的非药物性慢性肝损伤。
胆汁淤积型DILI一般在停药3个月-3年恢复;
少数患者病情迁延,可导致胆汁淤积性肝硬化,预后不良。
药物性急性/亚急性肝衰竭病死率高。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













这份分享有年头了,但仍有学习的意义
6
👍🏻
85
好
88
学习啦
86
#肝损伤#
99
#损伤#
53
#药物性#
65
很有临床指导意义
88
非常详细实用
94
学习了
77