Lancet haematol:感染COVID-19的血液恶性肿瘤患者的临床特征和不良预后相关因素
2020-08-14 QQY MedSci原创
新冠病毒仍在全球肆虐,严重危及了人们的健康和生命,肿瘤患者感染新冠病毒后的预后往。本研究旨在分析因COVID-19住院的血液恶性肿瘤成年患者的临床预后及相关风险因素。
几个关于COVID-19和血液恶性肿瘤的患者的小研究显示,这类患者人群的死亡率高。意大利COVID-19血液学联盟的目标是收集因COVID-19需要住院的血液恶性肿瘤成年患者的数据。该数据分析结果于近日发表在《柳叶刀·血液学》杂志上。
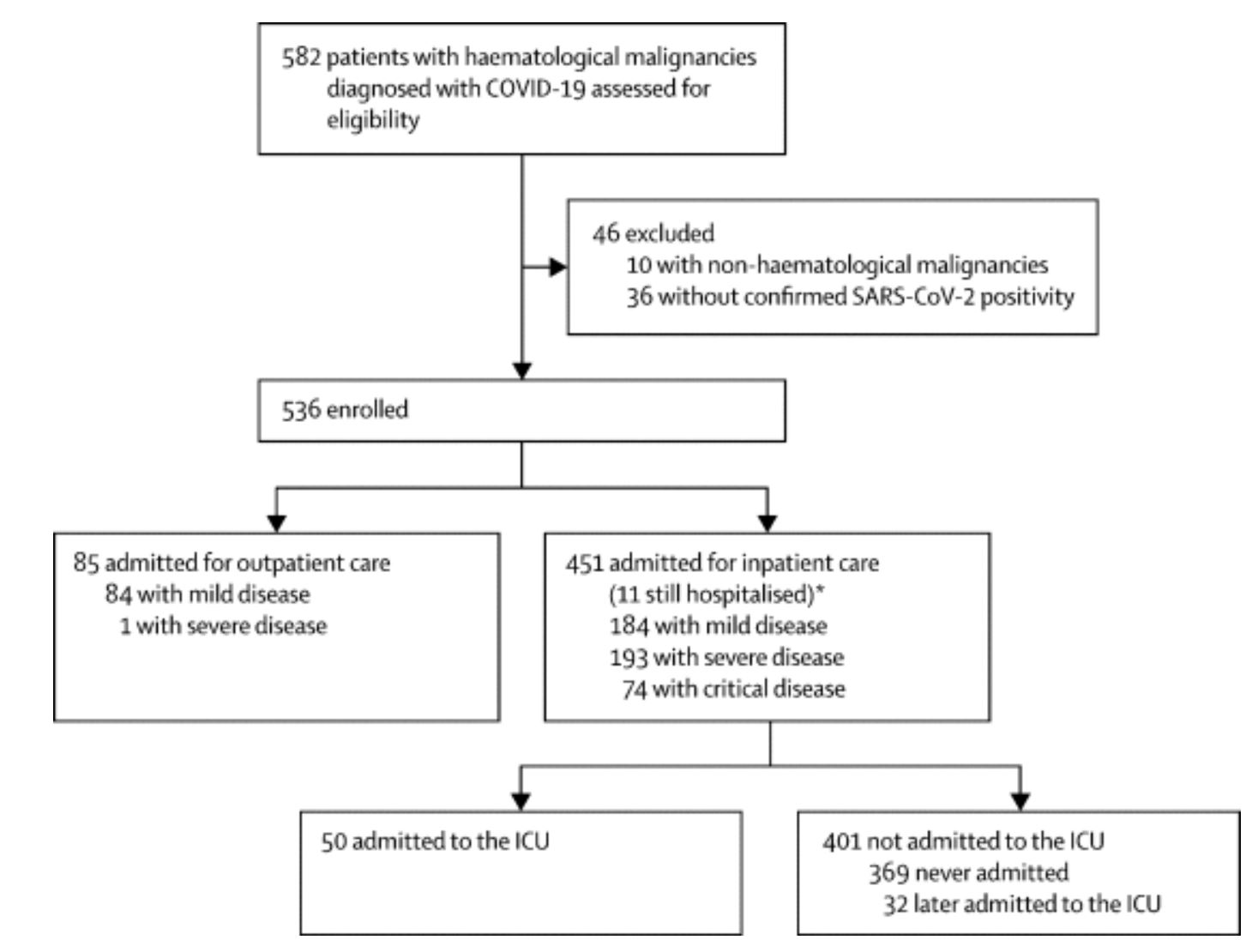
该研究是一个多中心的回顾性队列研究,纳入于2020年2月25日-5月18日期间住院的年满18岁的确诊COVID-19感染并有相关症状的血液恶性肿瘤患者。主要终点是死亡率和死亡率的潜在预测参数的评估。
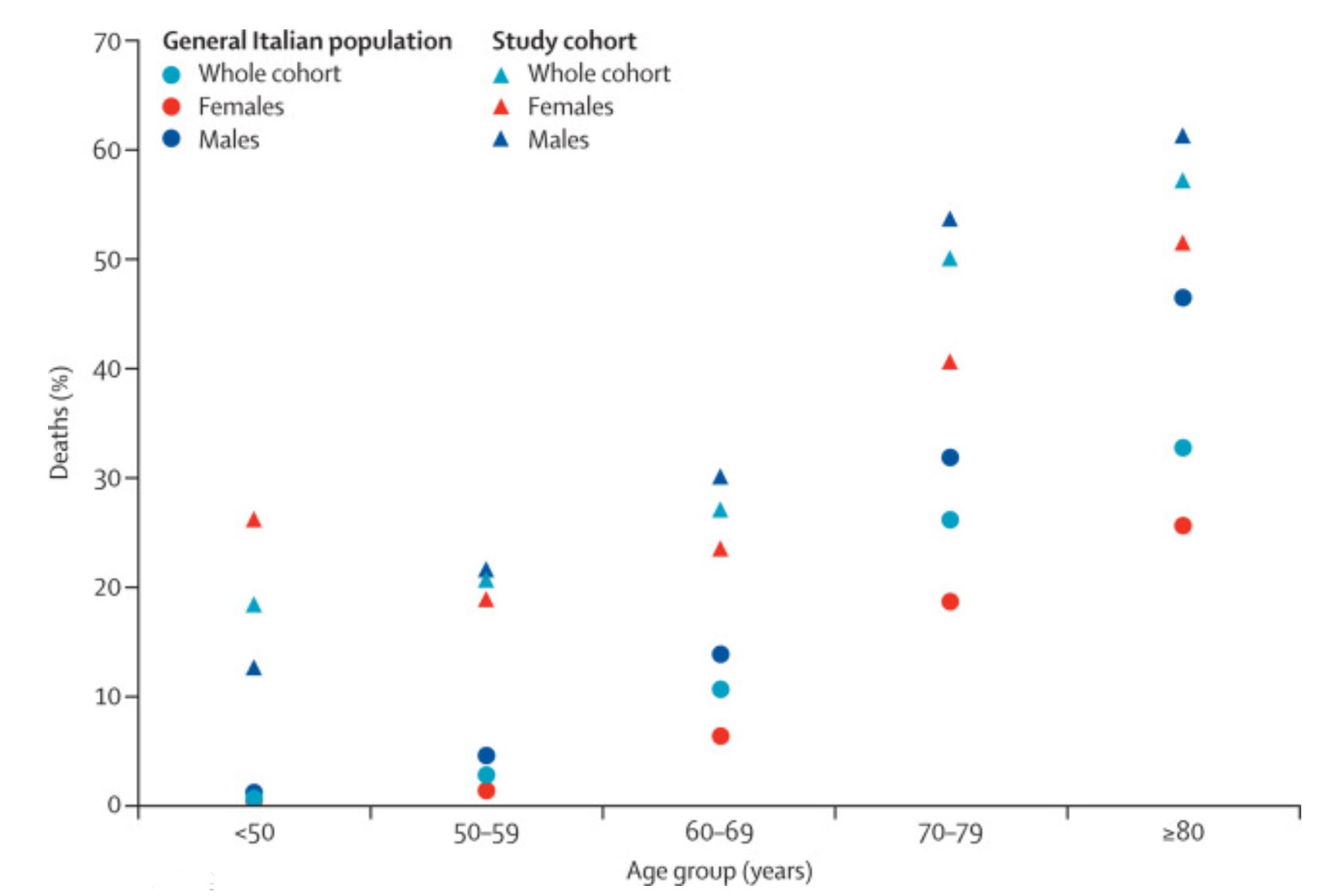
截止2020年6月22日,共纳入了536位患者,中位随访了20天(IQR 10-34),其中85位(16%)作为门诊患者管理。451位住院患者中有440位(98%)活着出院了或死亡。536患者中有198位(37%)死亡。与感染COVID-19的普通意大利人群相比,该研究整个队列的标准化死亡率为2.04(95%CI 1.77-2.34)。与非COVID-19感染的血液恶性肿瘤患者相比,该研究队列的标准化死亡率为41.3 (38.1–44.9)。年级大、进展期、确诊AML、惰性非霍奇金淋巴瘤、侵袭性非霍奇金淋巴瘤或浆细胞肿瘤和重度或危重型COVID-19均与总体预后更差有关。
该研究再次证明了,血液恶性肿瘤患者感染COVID-19后的预后比感染COVID-19的一般人或未感染COVID-19的血液恶性肿瘤患者的预后均更差。因COVID-19住院的血液恶性肿瘤患者的高死亡率突出表明,至少在有有效的疫苗接种或治疗策略之前,有必要采取积极的感染预防策略。
原始出处:
Francesco Passamonti,et al. Clinical characteristics and risk factors associated with COVID-19 severity in patients with haematological malignancies in Italy: a retrospective, multicentre, cohort study. The Lancet Haematology. August 13,2020.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#临床特征#
44
#Lancet#
56
#EMA#
43
#不良预后#
58
#肿瘤患者#
50
#相关因素#
59
#HAE#
37
顶刊就是不一样,质量很高,内容精彩!学到很多
56