PLOS MED:中风发病存在昼夜差异——夜间发病更容易出现的严重结果
2022-02-13 MedSci原创 MedSci原创
与日间发病的脑卒中相比,夜间发病的脑卒中具有更高的神经系统严重性,更频繁的END,以及更差的3个月功能结果。
尽管众所周知,上午发生不良心血管事件如卒中和心肌梗死有所增加,但关于卒中发病时间与短期/长期结果之间的关系只有少数相对较小的研究,结果也不一致。此外,这些研究往往没有考虑到缺血性卒中的亚型。
临床前数据表明,缺血性卒中的进展存在昼夜变化,非活动期(白天)的啮齿动物模型比活动期(夜间)的卒中发病时的细胞死亡和梗塞生长更为活跃。为了研究中风发病时间与人类缺血性中风的严重程度、早期神经系统恶化(END)和长期功能结局的关系,来自韩国的专家开展了相关研究,结果发表在PLOS MEDICINE杂志上。
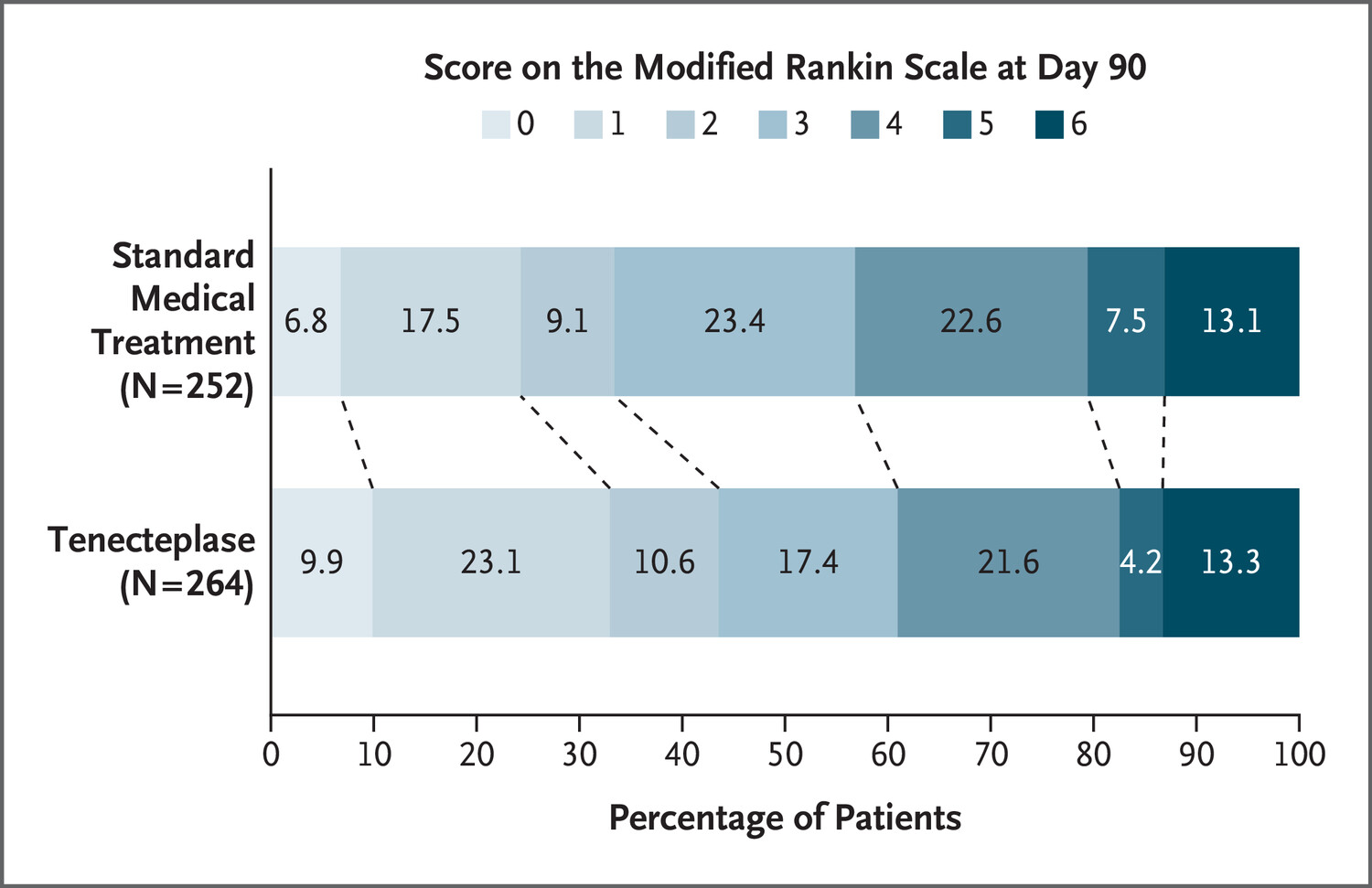
在2011年5月至2020年7月的一项韩国全国性多中心观察队列研究中,研究人员评估了昼夜节律对初始卒中严重程度(入院时NIHSS评分)、END和有利的功能结局(3个月mRS评分0-2与3-6)的影响。纳入了17461名患者,根据卒中发病时间分为2组(日间发病[06:00至18:00]与夜间发病[18:00至06:00]),按4小时间隔分为6组。
结果显示,在调整了包括年龄、性别、既往卒中、卒中前mRS评分、入院NIHSS评分、高血压、糖尿病、高脂血症、吸烟、心房颤动、卒中前抗血小板使用、卒中前他汀使用、血管再造、卒中发病季节以及发病至入院时间等协变量后,与日间发病的卒中相比,夜间发病的卒中更容易发生END(发病率为14. 4% vs 12.8%,P=0.006),且有利结局的可能性较低(OR=0.88[95%CI,0.79-0.98];P=0.03)。

当卒中发病时间按4小时间隔分组时,注意到呈现NIHSS评分的单调梯度,从06:00至10:00的低谷上升到02:00至06:00的高峰。18:00至22:00和22:00至02:00发病的卒中患者比06:00至10:00发病的卒中患者更可能出现END。在3个月时,良好功能结局的比率有一个单调的梯度,从06:00至10:00的高峰下降到22:00至02:00的低谷。
与日间发病的脑卒中相比,夜间发病的脑卒中具有更高的神经系统严重性,更频繁的END,以及更差的3个月功能结果。
参考文献:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言

















至北京时间2022年2月14日8时01分,
100
学习
81
学习了 谢谢
85
学习了
101
有意义,指导生活
78
#Med#
43