J Vasc Surg Venous Lymphat Disord:威廉亚洲官网 速递|急性静脉血栓栓塞临床研究——导管定向溶栓治疗深静脉血栓患者颅内出血的预测因子分析
2021-08-11 “Clinic門诊新视野”公众号 “Clinic門诊新视野”公众号
搜集从2005年1月至2013年12月,美国国家住院样本数据库识别的所有下肢近端或腔内深静脉血栓形成(DVT)的患者。采用多因素logistic回归分析,确定单纯抗凝治疗和CDT+抗凝治疗的DVT患者
尽管急性颅内出血(ICH)是导管定向溶栓(CDT)的罕见并发症,但仍是CDT使用相关的主要问题。在CDT背景下发生ICH的发生率和临床预测因素尚不清楚。Patrick Cherfan等进行的研究旨在探讨在接受CDT治疗的下肢或下腔静脉DVT的患者中ICH的独立预测因素和预后。该研究结果发表于2021年5月最新一期的Journal of Vascular Surgery: Venous and Lymphatic Disorders杂志。
研究目的
搜集从2005年1月至2013年12月,美国国家住院样本数据库识别的所有下肢近端或腔内深静脉血栓形成(DVT)的患者。采用多因素logistic回归分析,确定单纯抗凝治疗和CDT+抗凝治疗的DVT患者脑出血的临床预测因素。
研究结果
在138,049例下肢近端或下腔静脉DVT患者中,有7,119名(5.2%)接受了抗凝治疗和CDT。在仅接受抗凝治疗的患者中,ICH的发生率为0.2%,而使用CDT的患者ICH的发生率为0.7%(P<0.01)。在接受CDT治疗的患者中,51例(0.7%)发展为脑出血。在仅接受抗凝治疗的患者中,发生ICH的危险因素为卒中史,医院教学状况以及年龄>74岁(表1)。在接受CDT治疗的人群中ICH的独立预测因素是卒中史(优势比[OR]为19.4;95%置信区间[CI]为8.8-42.8;P<0.01),慢性肾脏病(OR为2.2;95%CI,1.1-4.7;P=0.03),年龄>74岁(OR,2.2;95%CI,1.2-4.3;P=0.02),男性(OR,1.8;95%CI,1.01-3.3;P=0.048;表2)。
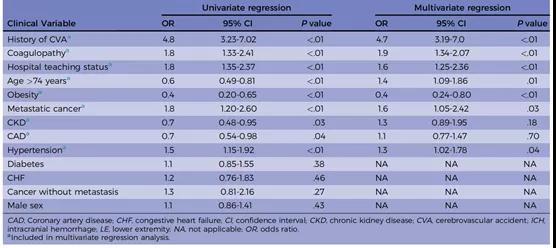
表1. 抗凝治疗组脑出血预测因素的单因素和多因素logistic回归分析
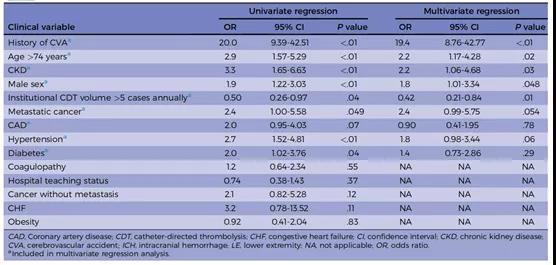
表2. 抗凝治疗加CDT组脑出血预测因素的单因素和多因素logistic回归分析
结 论
目前美国全国范围内的观察性研究结果显示,在接受CDT治疗的DVT患者中,发展为脑出血的独立预测因子是卒中史、慢性肾脏疾病、男性和年龄>74岁。
原始出处:
Lakhter V, Zack CJ, Brailovsky Y, et al. Predictors of intracranial hemorrhage in patients treated with catheter-directed thrombolysis for deep vein thrombosis. J Vasc Surg Venous Lymphat Disord. 2021;9(3):627-634.e2.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#静脉#
61
#Dis#
58
学习了
74
#静脉血#
56
#Disord#
51
#定向#
83
#ASC#
46
#预测因子#
44
#溶栓治疗#
85