J Neurosurg Spine:胸椎后纵韧带骨化在后路减压融合术后仍旧进展并增大
2014-11-30 王海强 丁香园
后纵韧带骨化为脊柱韧带的异位骨化,压迫脊髓而可引起脊髓病变。尽管文献中关于颈椎后纵韧带骨化的进展报道很多,关于胸椎后纵韧带骨化进展的情况,尚不明确。目前,对于胸椎后纵韧带骨化引起压迫症状的首选治疗为后路减压和固定融合,短期疗效好。前路减压技术要求高,并发症也高。 一般认为,脊柱内固定可减少脊髓压迫,进而通过消除动力效应和减少机械应力而抑制骨化。尽管后纵韧带骨化长期进展可抵消手术效果,但胸椎后纵韧
后纵韧带骨化为脊柱韧带的异位骨化,压迫脊髓而可引起脊髓病变。尽管文献中关于颈椎后纵韧带骨化的进展报道很多,关于胸椎后纵韧带骨化进展的情况,尚不明确。目前,对于胸椎后纵韧带骨化引起压迫症状的首选治疗为后路减压和固定融合,短期疗效好。前路减压技术要求高,并发症也高。
一般认为,脊柱内固定可减少脊髓压迫,进而通过消除动力效应和减少机械应力而抑制骨化。尽管后纵韧带骨化长期进展可抵消手术效果,但胸椎后纵韧带骨化在脊柱固定后是否进展,尚不明确。
日本东京大学医学院骨科的学者进行了一项随访研究,提示胸椎后纵韧带骨化在后路减压融合术后仍旧进展并增大,文章于2014年11月发表在J Neurosurg Spine上。
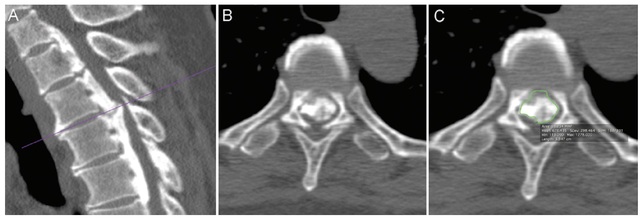
该研究纳入9例胸椎后纵韧带骨化行后路减压、内固定融合的连续病例,随访时间至少3年。对手术前和最后随访时胸椎的薄层CT进行分析,在CT矢状面重建图像中确定胸椎压迫最明显的节段,并在以上确定的平面的轴位图像上,采用医学数字图像和交流DICOM软件,测量骨化区域面积(图1)。

图1 A:在CT矢状位重建图像上选定突出最明显平面(横线);B:选定平面的横截面;C:使用软件功能(绿色框)计算骨化区域面积。
术前、术后出院时及最终随访时脊髓病变的严重程度采用JOA评分确定下肢肌力功能。
结果显示,所有患者,后纵韧带骨化面积增加,从手术前的83.6±25.3mm2增加到最终随访时的114.8±32.4 mm2+。神经功能并未因后纵韧带骨化进展而加重。
以上结果提示,胸椎后纵韧带骨化的面积,在后路固定后,依然增大。尽管脊柱局部活动度降低,后纵韧带骨化并未缩小或停止进展。对于胸椎后纵韧带骨化的患者,医生应当注意到其进展的情况。
本研究首次报道了胸椎后纵韧带骨化在脊柱固定后的进展,其潜在的机制尚不明确,有待进一步研究。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#Spine#
33
#后纵韧带#
42
脊柱融合术中是否使用BMP后的骨不连的发生率无统计学差别
140
#ROS#
69
#胸椎#
48
#韧带#
44
#融合#
55
#融合术#
0