化召辉:高龄(≥80岁)颅外颈动脉狭窄治疗选择
2021-01-31 《门诊》杂志 门诊新视野
颅外颈动脉狭窄可引起脑卒中和短暂性脑缺血发作,严重威胁患者生命。此外,随着老龄化进程,高龄颈动脉狭窄患者群体逐渐庞大,对于这一群体选择何种治疗方式最合理是血管外科医师亟待解决的问题。
颅外颈动脉狭窄可引起脑卒中和短暂性脑缺血发作,严重威胁患者生命。此外,随着老龄化进程,高龄颈动脉狭窄患者群体逐渐庞大,对于这一群体选择何种治疗方式最合理是血管外科医师亟待解决的问题。2020年11月27~28日,在2020中国脑卒中大会颈动脉狭窄外科干预手术直播论坛上,来自郑州大学第一附属医院的化召辉教授在科主任李震教授的指导下就高龄(≥80岁)颅外颈动脉狭窄治疗选择作了精彩的演讲。
颈动脉狭窄手术治疗现状
颈动脉狭窄的治疗方式药物治疗和手术治疗,其中手术方式包括颈动脉内膜剥脱术(CEA)、颈动脉支架成形术(CAS)以及经颈动脉血管重建术(TCAR)。至今,CEA手术已应用于人体数十年,虽然有一定的心梗、颅神经损伤的风险,但能够确切的改善患者的症状、解除狭窄病灶,最大程度的降低卒中风险,被用于大部分颈动脉狭窄患者的治疗。CAS创伤更低、手术不良事件更少,但是30天卒中风险更高,目前约14%的患者接受CAS手术。
近年来,国内外颈动脉狭窄治疗威廉亚洲博彩公司 对症状性颈动脉狭窄的CEA手术推荐级别均为IA级。2017 ESVS威廉亚洲博彩公司 推荐多学科评估,就CEA或CAS的适应证和最佳治疗方案达成共识包括:
1)6个月内出现同侧颈动脉灌注区相关症状,狭窄程度为70%~99%的患者,推荐行CEA;狭窄程度为50%~69%的患者,可考虑行CEA;年龄>70岁,狭窄程度为50%~69%的患者,推荐行CEA,而非CAS;年龄<70岁,适于颈动脉血运重建的患者,可考虑将CAS作为CEA的替代疗法;
2)发病后14天内,拟行颈动脉血运重建的患者,更宜行CEA而非CAS;
3)狭窄程度50%~99%,合并卒中或TIA逐渐加重的患者,应考虑立即行CEA(24 h内最佳)。
年龄对颈动脉血流重建的影响
既往研究显示CAS在年轻患者中卒中风险相对较低,在年长患者中卒中风险相对较高。而年龄对CEA的卒中风险影响不明显,但心梗及神经损伤高于CAS。而当前新兴的TCAR技术在高龄且外科风险高的患者中显示出了较好的疗效。
2011年,Voeks 等发现CAS的首要终点不良事件随年龄增加,每十岁增加1.77倍;但是年龄对CEA术后结果无明显差异,且有/无症状及性别对年龄导致的差异无影响。Dakour-Aridi等就卒中/死亡风险的影响因素进行评分,评分越高CAS术后30天卒中/死亡风险越高,结果显示80岁以上CAS术后卒中/死亡风险显着升高(图1),表明患者年龄对颈动脉血流重建存在一定的影响。
一项回顾性研究纳入473例80岁以上颈动脉狭窄患者,分为CEA组(n=178)和CAS组(n=295),分析了术后30天内的并发症及术后5年的生存情况。结果显示80岁以上患者群体,CAS和CEA术后30天内心梗发生率分别为0.3%和2.8%,具有显着差异;死亡、TIA及卒中发生率无显着差异。CAS术后5年生存率显着优于CEA,但是5年的无卒中发生情况劣于CEA,主要原因可能是CEA术后心梗发生率高对生存率的影响作用。
ROADSTER-2研究提示在高龄患者(>80岁)中,TCAR组的死亡、同侧卒中、卒中等事件的发生率均显着低于CAS组。
一项对比TCAR、CAS及CEA治疗高龄患者疗效的研究,纳入了3,152例TCAR、10,381例TFCAS和61,650例CEA,不同年龄组TCAR与CEA的比较结果无显着差异。在80岁以上的患者中,与CAS组相比,TCAR组中风风险降低72%,中风/死亡风险降低65%,中风/死亡/心肌梗死风险降低76%。需要注意的是,在80岁以上无症状患者中,相较于CAS,TCAR的优势仅体现在降低卒中方面,而在有症状患者中,其优势在降低卒中、死亡方面均有体现。
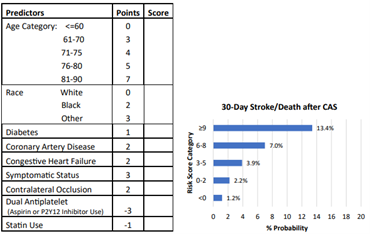
图1. CAS术后30天内卒中/死亡风险的影响因素评分
颈动脉手术的影响因素
影响颈动脉手术的独立危险因素包括患者个人因素(病变性质、位置、年龄、伴随疾病)、术者经验、支架类型及脑保护、团队协作以及手术入路方式。研究显示手术量≥20例/年的医院才能有效锻炼术者操作经验,提高手术疗效。此外,医疗机构及术者也会影响TCAR与CEA结果,在同一机构由同一位外科医师进行TCAR与CEA手术相比,中风、心梗和死亡率无明显差异。规范的训练及一定的手术量可以弥补不同手术方式在年龄差异中导致的结果偏差。
总 结
颈动脉重建的3种术式都有存在的价值,其中高龄是手术结果的危险因素之一。此外,病变性质、围术期管理及患者依从性也是重要考量因素。
CAS在高龄患者中卒中相对风险较高,CEA卒中风险与年龄差异无关,脑保护方法、药物及材料的进展会改变治疗模式。TCAR在高龄患者中显示出更安全的结果趋势,但术者经验、手术量及围术期管理对不同术式在年龄差异中导致的结果有明显影响。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言














学习
53
#颈动脉#
0
#治疗选择#
62
#高龄#
0
#动脉狭窄#
56