Neuromodulation:丘脑底核脑深部刺激幅度增加对帕金森病眼动抑制性控制的影响
2021-06-21 MedSci原创 MedSci原创
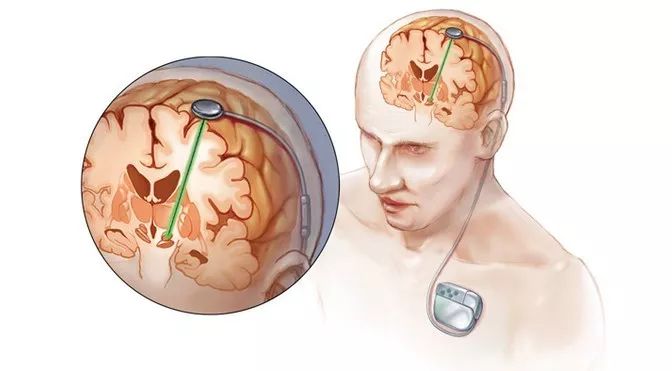
多种因素决定了丘脑底核脑深部电刺激(STN-DBS)治疗帕金森病(PD)的有效性。科学的病人选择和准确的引线安置为良好的结果奠定了基础。导线植入后,四个变量的编程最终决定刺激的有效性:识别导线上的最佳
多种因素决定了丘脑底核脑深部电刺激(STN-DBS)治疗帕金森病(PD)的有效性。科学的病人选择和准确的引线安置为良好的结果奠定了基础。导线植入后,四个变量的编程最终决定刺激的有效性:识别导线上的最佳接触(或节段)、频率、脉冲宽度和振幅 。电信号的振幅是初始编程期间调整最多的参数,与其他参数的能量等效变化相比,对改善运动症状的影响最大。通过电压(V)或电流(mA)控制的DBS系统增加振幅,导致注入电极接触周围组织的电流增加。系统研究电压效应的研究表明,3或4V是改善运动症状(如震颤、强直和运动迟缓)最有效的刺激幅度。刺激幅度的进一步增加可能导致负面副作用。此外,与低振幅相比,高振幅刺激可能诱发或加重PD的其他症状,如步态冻结 。

为了探讨刺激幅度与认知之间的关系,本研究探讨了刺激幅度对动眼神经控制的一个特定认知方面,即抑制性控制的影响。据williamhill asia 所知,这是第一次评估刺激幅度对抑制性控制等认知测量的影响的研究,在本研究中,评估了双侧STN-DBS振幅对反痉挛任务中正向眼跳错误率的影响。 评估了双侧STN-DBS振幅对正确的抗痉挛试验潜伏期的影响,以深入了解错误的可能机制。
本研究中招募了15名接受双侧STN-DBS治疗帕金森病的患者。在15名参与者中,有5人无法完成数据收集。在受试者服用药物和STN-DBS时进行蒙特利尔认知评估(MoCA)。为了证实受试者有治疗上有益的STN-DBS,在受试者在基线下停用/停用STN-DBS,进行了运动障碍学会-统一帕金森病评定量表(MDS-UPDRS)第三部分运动检查。参与者在6个不同的刺激幅度(0、1、2、3、3.5和4V或mA)下执行抗癫痫任务(例如,左侧STN刺激器设置为4V,右侧STN刺激器设置为4V)。频率、脉冲宽度和有效接触保持在基线临床设置。williamhill asia 调整了8名受试者的电压(美敦力公司,明尼苏达州明尼阿波利斯市)和2名受试者的电流。
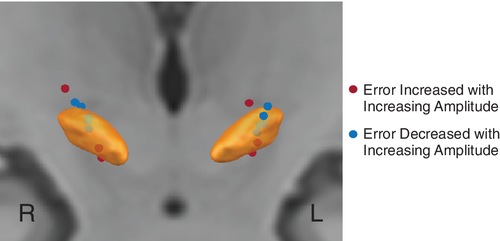
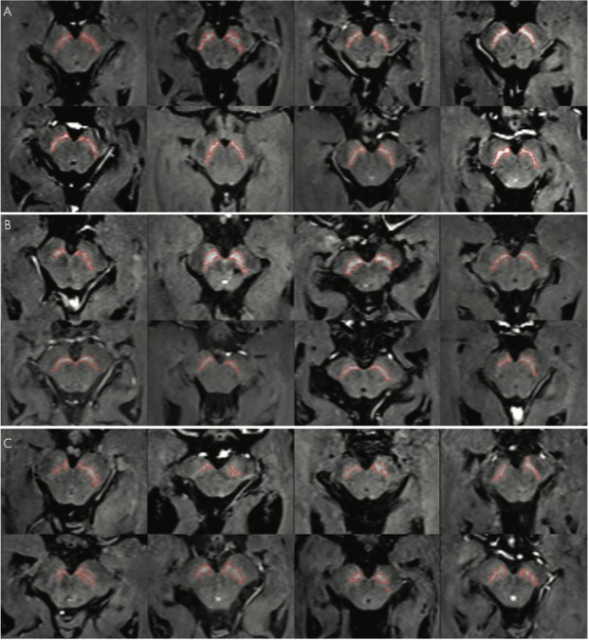
电极触点和STN
10名参与者中的5名进行了术前MRI和术后CT或MRI图像。所有5名有影像和4个接触电极的受试者术前均进行了T1加权MPRAGE,其中4名受试者进行了T2加权turbo自旋回波序列。术前影像学检查需要对术后影像学进行登记。五分之四的受试者进行了术后CT检查,一名受试者进行了术后T1加权平均值检查。
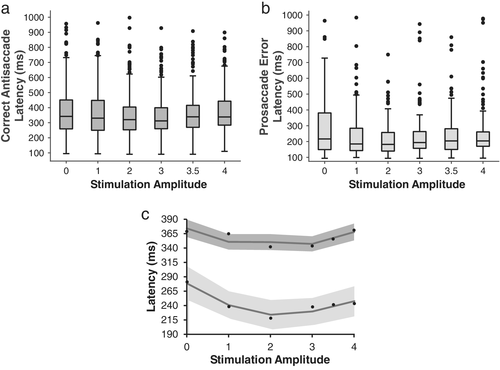
刺激幅度对眼跳潜伏期的影响
随着STN-DBS振幅的增加,抑制痉挛任务的正向眼跳错误率也随之增加。当刺激幅度大于3V或3mA时,健康年龄匹配错误率约为对照组的3倍。此外,结果表明,电极位置影响抑制控制的中断,但这种关系随刺激幅度而改变。随着刺激幅度的增加,正向眼跳错误率的增加并不依赖于潜伏期的减少。数据表明STN-DBS振幅在抑制控制和运动症状改善中起着关键作用。刺激幅度和主动接触的位置是影响运动症状改善和抑制性控制损伤的关键因素。这些信息对于临床医生优化刺激设置非常重要,以便在减少或消除认知副作用的同时保持运动益处。
Munoz, M.J., Goelz, L.C., Pal, G.D., Karl, J.A., Verhagen Metman, L., Sani, S., Rosenow, J.M., Ciolino, J.D., Kurani, A.S., Corcos, D.M. and David, F.J. (2021), Increased Subthalamic Nucleus Deep Brain Stimulation Amplitude Impairs Inhibitory Control of Eye Movements in Parkinson's Disease. Neuromodulation: Technology at the Neural Interface.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#丘脑#
72
#丘脑#
45
受益匪浅
70
好
76
已读,真是受益匪浅呀。
72