Radiology:磁共振扩散峰度成像与人工智能的结合:预测直肠癌对新辅助放化疗的反应
2021-06-10 shaosai MedSci原创
多项研究表明,新辅助放化疗(NCRT)可有效降低局部晚期直肠癌的分期,并在大约20%的患者中达到病理完全缓解(pCR)。
 多项研究表明,新辅助放化疗(NCRT)可有效降低局部晚期直肠癌的分期,并在大约20%的患者中达到病理完全缓解(pCR)。患者对NCRT的反应情况对于预后和治疗方案的选择尤为重要。目前,治疗反应主要是通过手术后的组织病理学评估进行确定,包括确定治疗后的病理T分期和N分期、环周切缘状态和肿瘤消退分级(TRG)。然而,若可做到对这类特征进行术前评估则对手术方案的制定意义重大。
多项研究表明,新辅助放化疗(NCRT)可有效降低局部晚期直肠癌的分期,并在大约20%的患者中达到病理完全缓解(pCR)。患者对NCRT的反应情况对于预后和治疗方案的选择尤为重要。目前,治疗反应主要是通过手术后的组织病理学评估进行确定,包括确定治疗后的病理T分期和N分期、环周切缘状态和肿瘤消退分级(TRG)。然而,若可做到对这类特征进行术前评估则对手术方案的制定意义重大。
扩散加权成像和T2加权成像的结合在反应评估中显示出一定的优势,但是据williamhill asia 所知,准确的术前治疗反应评估系统尚待开发。多项研究表明,扩散峰度MRI在评估肿瘤状态方面有较高的优势,其衍生出的参数Kapp反映了肿瘤环境非高斯扩散行为,而Dapp校正了非高斯效应后的正态扩散系数。与标准的单指数扩散加权成像分析相比,扩散峰度MRI提供了更多关于组织结构的信息,从而为放射科医生提供了更多深入了解组织特征的机会。
近日,发表在Radiology杂志的一项研究开发并验证了一种基于扩散峰度和T2加权MRI的DL方法来预测直肠癌对新辅助治疗的反应,提供了一个非侵入性反应评估模型以协助临床制定最佳的治疗方案及预测患者预后。
在本项前瞻性研究中,纳入的经病理证实为局部晚期直肠癌(≥cT3或N +)患者在进行术前化疗时均接受了基线MRI扫描,并按时间顺序分为308个训练样本和104个测试样本。构建DL模型主要用于预测病理完全缓解(pCR),其次评估肿瘤消退分级(TRG) (TRG0和TRG1 vs TRG2和TRG3)和T分期的下降程度。同时比较了扩散峭度MRI参数和放射科医生的主观评价。
本研究共纳入了383名参与者(平均年龄57岁±10岁[标准差];229位男性),其中290人在训练组,93人在测试组。试验队列pCR模型的受试者工作特征曲线下面积(AUC)为0.99,高于评分者1和2的AUC(分别为0.66和0.72,P均< .001)。DL模型在预测TRG方面的AUC为0.70,在预测T分期下降方面的AUC为0.79 。对于诊断效能最佳的扩散峰度MRI参数,DL模型预测pCR方面的AUC优于单独的AUC(Dapp值,AUC = 0.76)。与应用DL模型预测pCR(2.2%)相比,放射科医生的主观评估产生了更高的错误率(26.9%和24.8%);而在DL模型的辅助下,放射科医师的错误率明显降低(12.9%和14.0%)。
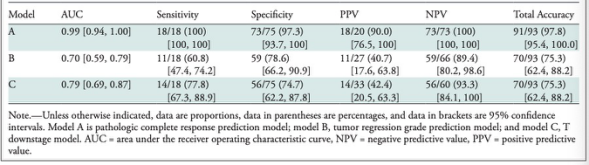
表 试验队列中局部晚期直肠癌患者治疗反应预测的模型表现。
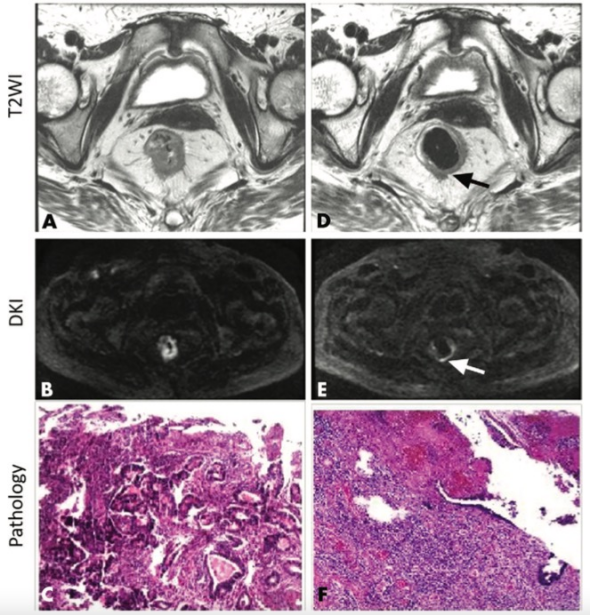
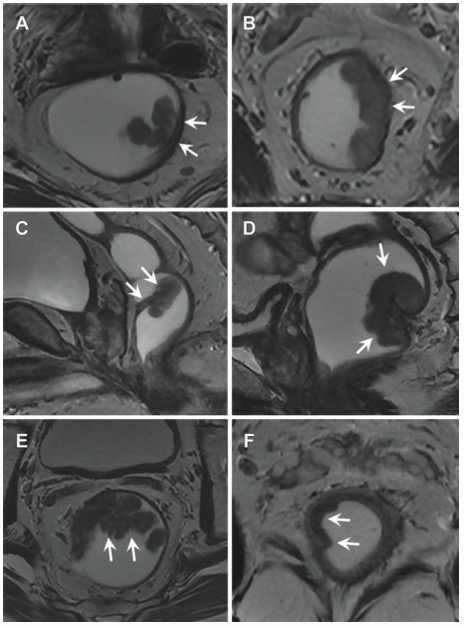
图 62岁,女性直肠癌患者,新辅助放化疗(NCRT)前后的T2WI (T2WI)、弥散峰度(DKI)和病理图像。NCRT前,(A)T2WI和(B)DKI图像显示肿瘤位置在直肠壁内1-9点钟位置。(C)结肠镜活检标本显示为直肠腺癌。NCRT后,(D)T2WI(箭头)和(E)DKI图像显示明显的肿瘤消退(箭头),仅显示直肠壁内3-6点钟位置的肿瘤残留。放射科医生的主观评价为非病理完全反应(pCR),即使深度学习模型诊断为pCR。(F)手术后的病理分析显示该患者为pCR。
本研究使用新辅助放化疗前后的扩散峰度MRI成像建立了一个基于深度学习的病理完全反应(pCR)预测模型,并在试验队列中取得了优异的诊断效能。同时研究发现,在深度学习模型的辅助下,放射科医师对pCR的主观评价表现得到了显著提高,这提示该模型可为临床常规pCR评价提供有效的诊断参考。
原文出处:
Xiao-Yan Zhang,Lin Wang,Hai-Tao Zhu,et al.Predicting Rectal Cancer Response to Neoadjuvant Chemoradiotherapy Using Deep Learning of Diffusion Kurtosis MRI.DOI:10.1148/radiol.2020190936
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#扩散峰度成像#
54
#辅助放化疗#
0
#新辅助#
36
#放化疗#
39
#磁共振#
39
#新辅助放化疗#
46
在深度学习模型的辅助下,放射科医师对pCR的主观评价表现得到了显著提高,这提示该模型可为临床常规pCR评价提供有效的诊断参考
72