Cell Metab:给二甲双胍跪了!科学家证实二甲双胍能抑制雾霾引起的动脉血栓,预防心血管疾病的发生
2018-10-17 奇点糕 奇点网
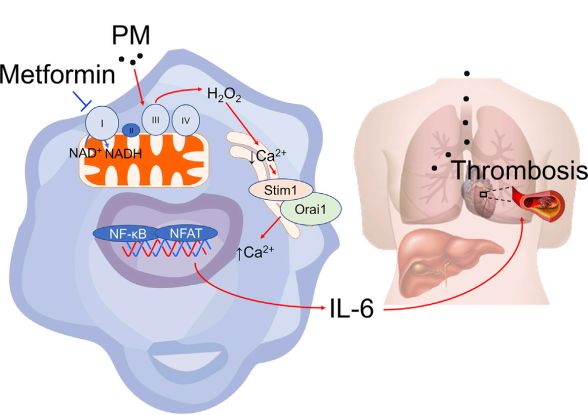
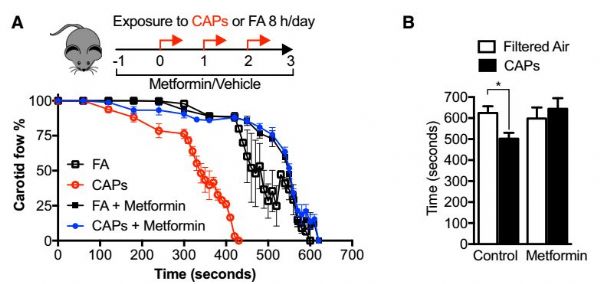
最近,美国西北大学的Scott Budinger教授带来了一个振奋人心的消息!他领导的团队在小鼠中证实,二甲双胍能预防雾霾引起的炎症,阻止免疫细胞释放一种危险分子到血液中,抑制动脉血栓的形成,从而降低心血管疾病的发病风险!

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#二甲双胍能#
60
#Cell#
45
#动脉血#
48
#MET#
59
#Meta#
43
非常不错的临床经验,学习了,值得借鉴,受益匪浅,感谢分享!
94
#CEL#
58
#雾霾#
55
#血管疾病#
53
#动脉血栓#
61