European Radiology:如何早期识别肺间质性疾病未来的病情进展?
2022-08-11 shaosai MedSci原创
最近有研究表明,正常密度的肺组织通气时异常高的气量变化与未来肺段容积的减少和肺平均密度的增加相关
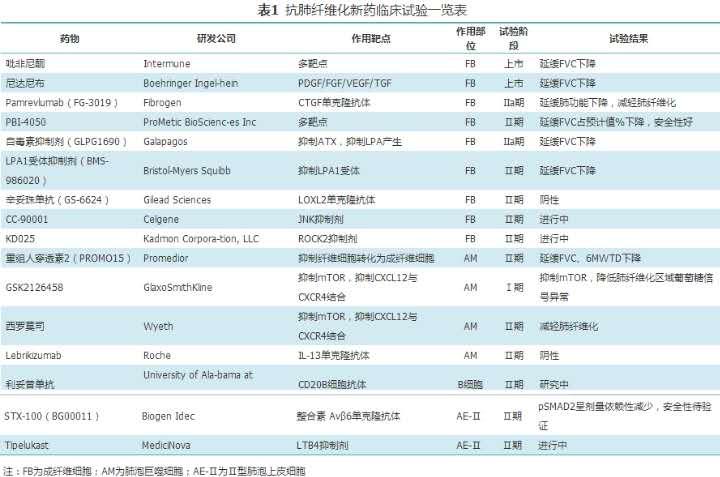
 特发性肺纤维化(IPF)是一种慢性、不可逆转的疾病,预后不良,诊断后中位生存期为3年,死亡率甚至超过许多癌症。抗研究发现,纤维化药物治疗可以显著减缓一部分患者的疾病进展,最近也被批准用于非特发性的进展性纤维化类型。目前的治疗指征包括功能下降(基于肺功能测试,PFT)、临床症状增加和CT上纤维化在特定时间段内的进展。
特发性肺纤维化(IPF)是一种慢性、不可逆转的疾病,预后不良,诊断后中位生存期为3年,死亡率甚至超过许多癌症。抗研究发现,纤维化药物治疗可以显著减缓一部分患者的疾病进展,最近也被批准用于非特发性的进展性纤维化类型。目前的治疗指征包括功能下降(基于肺功能测试,PFT)、临床症状增加和CT上纤维化在特定时间段内的进展。
最近有研究表明,正常密度的肺组织通气时异常高的气量变化与未来肺段容积的减少和肺平均密度的增加相关,这两者都被认为是纤维化结构变化的可量化的形态学指标。相应地,在异常高通气量和FVC下降之间也有相关性。然而,这些相关性是针对整个肺部计算的,没有研究评估肺部区域层面的空间关系。
近日,发表在European Radiology杂志的一项研究探讨了基线CT时区域通气量增加与IPF患者后续CT扫描的形态学变化之间的空间对应关系,这一发现将有助于早期识别有发生纤维化风险的肺实质,从而可以实现对潜在疾病进展的前瞻性评估。
本项回顾性研究在2016年9月至2020年11月的两个时间点进对所有参与者行了CT扫描。基线通气量被分为四个类别,从低、正常到中度和严重增加(C1-C4)。在相应的体素中调查了基线通气量与随访时体积和密度变化之间的相关性。每个通气量类别的密度和容积变化的差异的显著性采用配对t检验,其显著性水平为p≤0.05。对正常(NAA)和高衰减区(HAA)分别进行分析。
研究组由41名患者组成(73±10岁,36名男性)。在NAA和HAA中,与通气正常的区域(C2,P<0.001)相比,基线时通气严重增加的区域(C4)出现了明显的密度增加和体积损失。在HAA中,与NAA相比,形态学上的变化更具有异质性。

图 三个病例示例。上行显示基线吸气量(1),基线时的区域通气量(2),基线时的区域通气量由不同颜色编码(3)标记为四个类别。绿色表示基线通气量低至正常的区域(C2),而橙色(C3)和深红色(C4)分别表示基线通气量正常至中度和严重增加的区域。每张图的底排显示了与基线CT的后续吸气扫描(4)、相应的区域密度(5)以及再次与基线呼气扫描翘曲的区域容积变化图像(6)。(1)和(4)中的彩色编码标尺代表HU值,在(2)中代表标准化区域通气值,在(5)中代表HU变化,在(6)中代表体积变化的%值,在(2)中代表标准化区域静脉通气值,在(5)中代表HU变化,在(6)中代表体积变化的%
基于体素的研究分析表明,区域通气量和形态学变化在空间上是一致的。具有病理性高通气量的区域可以作为基线CT中风险组织的指标,随着时间的推移发展出结构性变化可提示纤维化的进展。
原文出处:
Sarah C Scharm,Cornelia Schaefer-Prokop,Moritz Willmann,et al.Increased regional ventilation as early imaging marker for future disease progression of interstitial lung disease: a feasibility study.DOI:10.1007/s00330-022-08702-w
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#病情#
65
#间质性#
58
#PE#
61
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
52