Blood:I期临床试验:依鲁替尼联合帕博西尼可有效治疗套细胞淋巴瘤
2019-02-08 MedSci MedSci原创
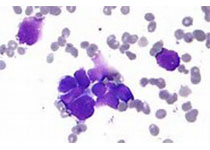
依鲁替尼单药用于既往治疗过的套细胞淋巴瘤(MCL)可获得治疗活性;但是,近一半患者在第一年会治疗失败。Peter Martin等人既往发现口服特异性的CDK4/6抑制剂palbociclib(帕博西尼)诱导的G1早期细胞周期阻滞延长,可克服人原发性MCL细胞和表达野生型BTK的MCL细胞系对依鲁替尼的耐药性。进而开展一I期临床试验评估帕博西尼联合依鲁替尼用于既往治疗过的套细胞淋巴瘤的剂量、安全性和
2014年8月-2016年6月,共招募了27位患者(21位男性、6位女性)。最大耐受剂量:依鲁替尼560mg/日+帕博西尼100mg/日,连续用药21天,28天一疗程。剂量限制性毒性是3级丘疹。最常见的3-4级毒性包括中性粒细胞减少(41%)、血小板减少(30%)、高血压(15%)、发热性中性粒细胞减少(15%)和肺炎(11%)。
中位随访25.6个月,总体和完全缓解率分别是67%和37%,2年无进展存活率为59.4%,2年缓解持续率为69.8%。现已开展II期的多中心临床试验进一步深入研究。
Peter Martin,et al.A phase I trial of ibrutinib plus palbociclib in previously treated mantle cell lymphoma. Blood 2019 :blood-2018-11-886457; doi: https://doi.org/10.1182/blood-2018-11-886457
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#细胞淋巴瘤#
45
#I期临床试验#
50
#I期临床#
51
#帕博西尼#
57
#有效治疗#
51