Keytruda联合PARP抑制剂III期临床试验失败!默沙东终止研究
2022-04-02 网络 网络
前列腺癌是男性第二大常见癌症,并且与显著的死亡率相关。前列腺癌的发展通常由雄激素驱动,包括睾酮。在mCRPC患者中,尽管使用了雄激素剥夺疗法来阻断雄激素的作用,但前列腺癌仍会生长并扩散到身体其他部位。
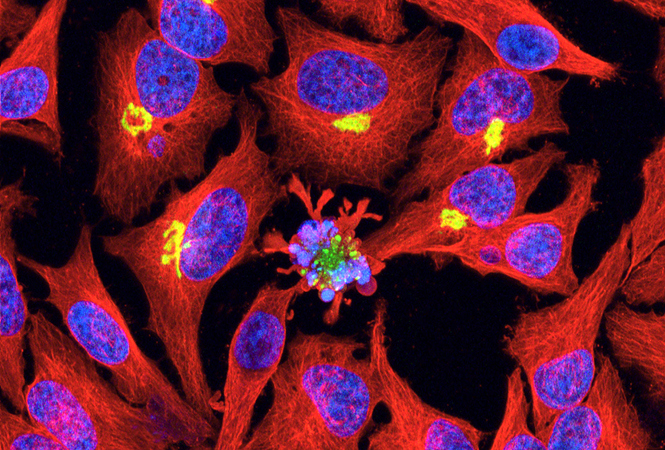
前列腺癌是男性第二大常见癌症,并且与显著的死亡率相关。前列腺癌的发展通常由雄激素驱动,包括睾酮。在mCRPC患者中,尽管使用了雄激素剥夺疗法来阻断雄激素的作用,但前列腺癌仍会生长并扩散到身体其他部位。大约10-20%的晚期前列腺癌患者将在五年内发展为CRPC,其中至少84%的患者在确诊为CRPC时已发生转移。确诊为CRPC没有转移的患者,33%可能在两年内发生转移。
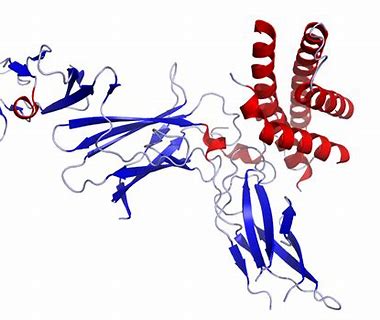
3 月 15 日,默沙东宣布 PD-1 单抗 Keytruda(帕博利珠单抗)与 PARP 抑制剂 Lynparza(奥拉帕利)联合疗法用于化疗和阿比特龙或恩杂鲁胺治疗后进展的转移性去势抵抗性前列腺癌(mCRPC)患者的 III 期临床 KEYLYNK-010 研究在中期分析中未能达到 OS 和放射影像学 PFS(rPFS)双重主要终点,并且还与 3-5 级不良事件发生率的提高相关。基于这一结果,默沙东将终止这项临床试验。

独立数据监测委员会 (DMC) 审查的中期分析数据显示,与对照组醋酸阿比特龙或恩杂鲁胺相比,Keytruda联合Lynparza并没有在总生存期(OS)方面显示出益处,OS是该研究的双重主要终点之一。该试验的另一个双重主要终点,影像学无进展生存期 (rPFS),在早期的中期分析中进行了评估,与对照组相比也没有表现出改善。相反,与对照组相比,联合用药组3-5级不良事件和药物相关严重不良事件发生率更高。
肿瘤领域,本月ORIC也在完成两项Ib期研究数据的中期分析后,决定停止ORIC-101的开发,原因是治疗并没有表现出足够的临床活性。此外,Silverback Therapeutics基于SBT6050在血清和肿瘤内暴露以及药效学标志物中观察到剂量反应,包括在治疗后从患者收集的组织活检中证明的免疫激活数据,以及SBT6050表现的单药有限抗肿瘤活性和细胞因子相关的不良事件限制与帕博利珠单抗的联合使用等,决定终止免疫刺激偶联药物SBT6050(HER2-TLR8)和SBT6290(Nectin4-TLR8)的临床研究。
非肿瘤领域,Avalo Therapeutics基于AVTX-007缺乏临床疗效信号,也决定终止进一步开发;Revelation Biosciences公布了鼻内给予REVTx-99a用于H3N2 流感预防性治疗的IIb期 RVL-VRL01研究中期统计分析结果,数据显示也未达到其主要疗效终点。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#III#
0
#I期临床#
70
#抑制剂#
59
#I期临床试验#
72
#PARP抑制剂#
113
#II期临床试验#
65
#默沙东#
67
#II期临床#
105
#III期临床试验#
53
#III期#
64