Oncol Nurs Forum:癌症影响癌症患者家属的健康行为
2015-02-24 Jessie 译 MedSci原创
Normal 0 10 pt 0 2 false false false EN-US ZH-CN X-NONE
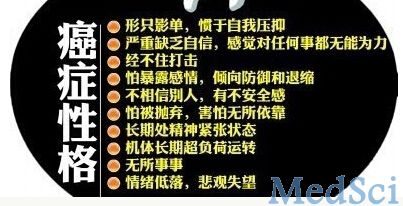
患癌症被认为是对患者进行健康教育、促进健康行为和保持健康生活方式的好时机。许多癌症患者在知道诊断后都想生活的更健康,健康的生活方式有助于缓和癌症治疗的副作用,防止发生其他的慢性疾病,并减轻现存慢性疾病对生活质量的影响。但关于癌症经历对患者家庭成员健康行为影响的研究较少,而家庭成员的健康行为有助于提高患者的健康水平。癌症治疗结束时被认为是进行健康行为干预的最佳时机。近来,美国的一项研究调查了癌症对患者家属健康行为的影响及影响家属采取健康行为的因素。 该研究在美国中西部一所综合性癌症中心招募了39名癌症患者的家属及50名癌症患者,癌症种类包括乳腺癌、直肠癌、头颈部肿瘤、肺癌及前列腺癌。调查时间是患者完成治疗前3周内。家属们完成了问卷调查、面对面或电话结构访谈。调查的内容包括健康饮食、躯体活动及戒烟的意愿、感知益处和信心,情绪困扰,家庭凝聚力、冲突和表达性(expressiveness)。 研究发现,癌症患者的家庭成员具有较高水平的健康饮食、每天进行30分钟的中度躯体活动的意愿、感知益处及信心(3.54~6.69,可能的范围为1~7)。癌症经历增加了患者家属对患癌危险性的
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#患者家属#
66
#Oncol#
52
mark
27
很不错学习了
120
好文章,超赞
81
#癌症患者#
43
不错的文章,学习了
129