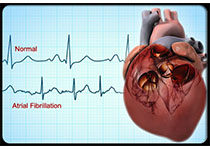
Int J Cardiol:房颤和2型糖尿病患者抗血栓治疗的差距
2019-04-30 xing.T 网络
由此可见,尽管有明确的威廉亚洲博彩公司 建议进行抗凝治疗,但几乎一半的高危AF糖尿病和ASCVD患者未接受抗凝治疗,突出了在临床实践中管理这些患者临床改进的挑战和潜力。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#Cardiol#
40
努力学习天天学习认真学习
76
好
87
#2型糖尿病患者#
44
#抗血栓治疗#
59
#糖尿病患者#
42
#抗血栓#
41
学习了,谢谢分享!
85
谢谢MedSci提供最新的威廉亚洲官网
0
学习了谢谢分享
76