JGH:长期使用质子泵抑制剂会增加骨质疏松症和髋部骨折的风险
2022-05-12 xuyihan MedSci原创
骨质疏松一般指骨质疏松症。 骨质疏松症(osteoporosis)是由于多种原因导致的骨密度和骨质量下降,骨微结构破坏,造成骨脆性增加,从而容易发生骨折的全身性骨病。
骨质疏松症是一种常见的疾病,其特点是患者骨量和微结构减少,导致骨质疏松性骨折的风险增加。 2017年,五个最大的欧盟国家(法国、德国、意大利、西班牙和英国)和瑞典新发生的骨质疏松性骨折的年度成本为375亿欧元。随着人口老龄化,骨质疏松症和骨质疏松性骨折预计将成为更严重的公共卫生问题。 质子泵抑制剂(PPIs)是细胞中H+/K+ATP酶的不可逆抑制剂,已被用于治疗胃酸相关疾病,如消化性溃疡病和胃食管反流病(GERD)。
随着PPIs使用的增加,出现不良反应和并发症的报告风险也更高,如胃肠道感染、胃底腺息肉、高胃泌素血症、急性和慢性肾脏疾病、骨质疏松性骨折和痴呆症。2006年的一项观察性研究首次报告了使用PPIs导致髋部骨折的风险增加。因此,目前还不清楚PPIs是否会导致骨质疏松症和/或髋部骨折。本项研究旨在评估转换为通用数据模型 (CDM) 的数据库中 PPI 的使用与骨质疏松症和髋部骨折风险之间的关系。
这是一项基于人群、倾向匹配的回顾性队列研究,包括年龄≥50 岁且被PPI治疗超过180天的患者被纳入研究。最后使用 Cox 比例风险模型比较了 PPI 新用户和其他药物新用户之间骨质疏松症和髋部骨折的发生率,并在电子健康记录 (EHR) 数据库中进行了荟萃分析。

在韩国国民健康保险局 (NHIS)-CDM 数据库中,研究人员发现长期使用PPI的人患骨质疏松症的风险更大(PPI 与非 PPI 组,28.42/1000人年VS 19.29/1000人年;HR,1.62;95% CI,1.22–2.15;P=0.001)。6 个 EHR 数据库的荟萃分析结果也显示出相似的结果(HR,1.57;95%[CI],1.28-1.92)。在髋部骨折分析中,PPI 的使用与 NHIS-CDM 数据库中的髋部骨折无显着相关性(PPI 与非 PPI 组,3.09/1000人年VS 2.26/1000人年;HR,1.45 ;95% CI,0.74–2.80;P=0.27)。然而,在 4 个 EHR 数据库的荟萃分析中,PPI 使用者髋部骨折的风险更高(HR,1.82;95% CI,1.04-3.19)。
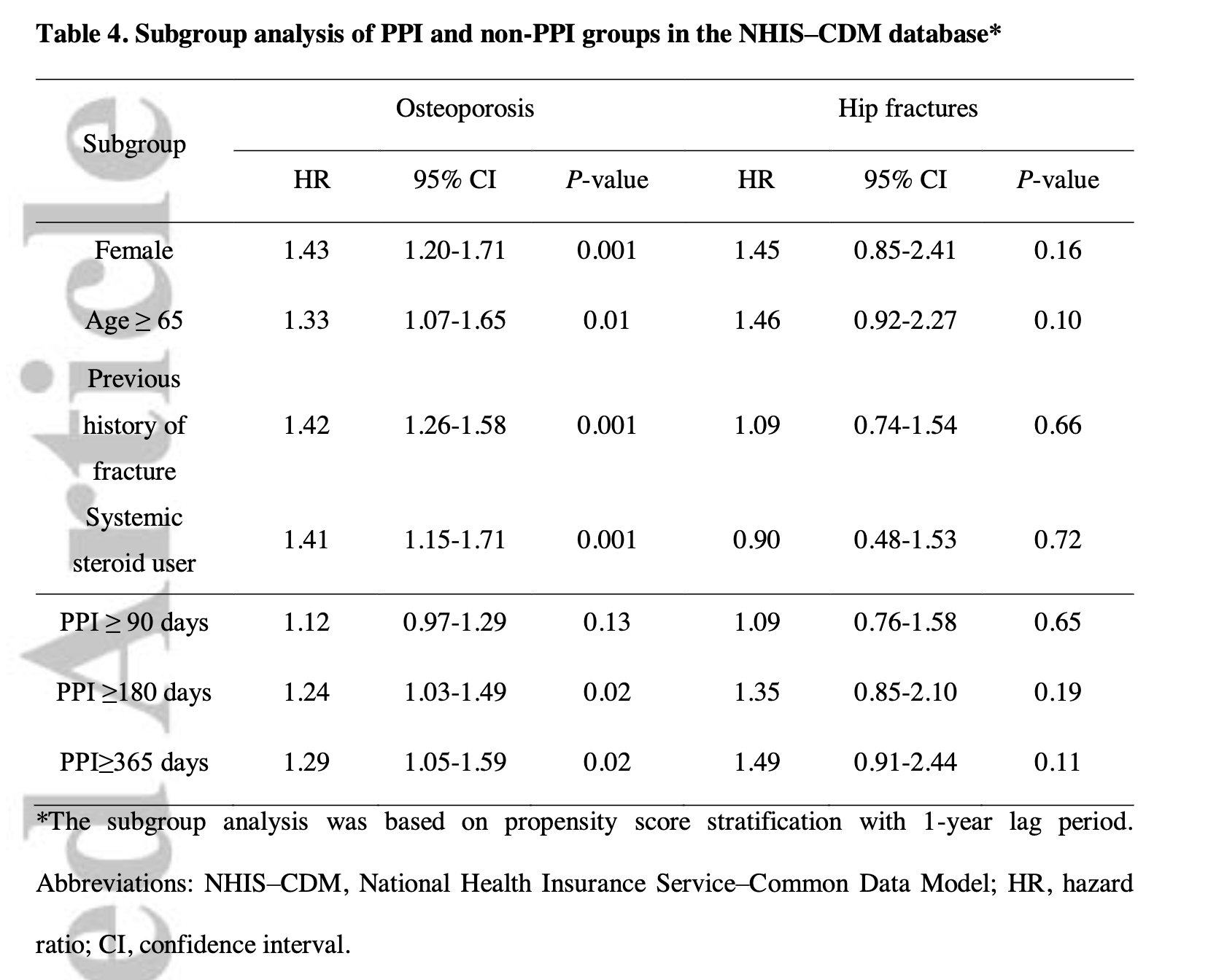
本项研究结果证实长期 PPI 与骨质疏松症显着相关,但髋部骨折的结果并不一致。可能需要基于更好的数据质量进行进一步研究。
原始出处:
Da Hee Park. Et al. Long-term proton pump inhibitor use and risk of osteoporosis and hip fractures: a nationwide population-based and multicenter cohort study using a common data model. Journal of Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#抑制剂#
61
#质子泵#
71
#长期使用#
63
#髋部#
63
#骨质#
63