ACS Nano:突破!科学家利用来自尿液的生物标志物进行早期癌症筛查
2017-03-09 佚名 生物谷
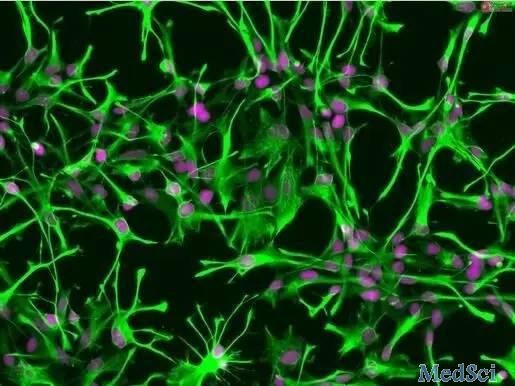
日前,来自韩国蔚山国家科学技术研究所的研究人员通过研究开发出了一种新技术,该技术能够有效在尿液或血液中有效鉴别出促进癌症发生的物质,相关研究刊登于国际杂志 ACS Nano 上。文章中,研究人员开发出了一种集成的离心微流体平台(Exodisc),这种设备能够对尿液中的胞外膜泡 (extracellular vesicles,EVs) 进行分离。研究人员希望这种技术或能用于临床设备中来检测尿液中基于
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#早期癌症#
62
#标志物#
49
#ACS#
44
#尿液#
47
#癌症筛查#
55
#生物标志#
38
#生物标志#
51