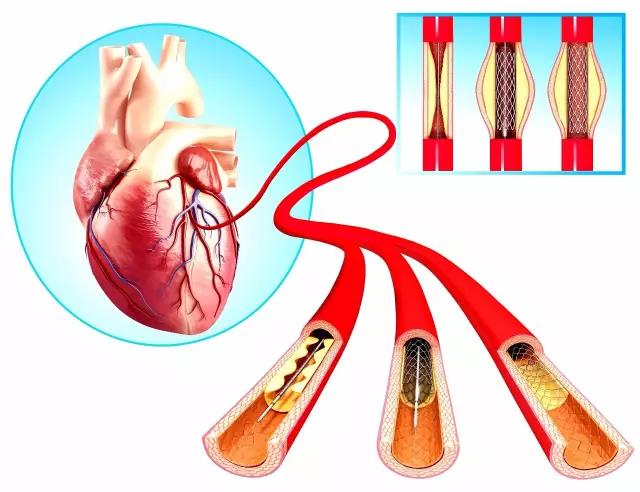
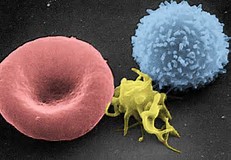
JACC:综述:抗血小板药治疗和预防冠状动脉粥样硬化
2017-11-03 吴刚 环球医学
2017年10月,意大利、葡萄牙和英国等国科学家在《J Am Coll Cardiol》发表了抗血小板药治疗和预防冠状动脉粥样硬化的综述
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#冠状动脉粥样硬化#
74
#粥样硬化#
58
#JACC#
62
#抗血小板药#
0
#ACC#
53