Eur Urol Focus:机器人辅助与腹腔镜前列腺根治术:多中心随机对照LAP-01试验的12个月结果
2022-04-02 AlexYang MedSci原创
比较了RARP和LRP在12个月的随访中的排尿能力、性交能力和肿瘤学结果。

此前,来自德国莱比锡大学等单位的研究人员进行的LAP-01试验证明了机器人辅助腹腔镜前列腺根治术(RARP)在3个月后的尿失禁方面优于传统腹腔镜前列腺根治术(LRP)。一般认为,RP患者即使在3个月后仍能继续恢复,特别是在尿失禁和性交能力方面。因此,12个月的功能性和肿瘤学数据对于比较不同手术方式的结果至关重要。
在本试验中,他们进一步比较了RARP和LRP在12个月的随访中的排尿能力、性交能力和肿瘤学结果。相关研究结果发表在《EUROPEAN UROLOGY FOCUS》期刊上。
在这项多中心、随机、患者盲目的对照试验中,德国四家医院转诊的前列腺根治术患者已3:1的比例被随机分配接受RARP或LRP。尿失禁作为患者报告的结果,被通过有效的调查问卷进行评估。次要终点包括性交能力和肿瘤学结果。研究人员通过双变量测试和多变量模型对数据进行统计分析。
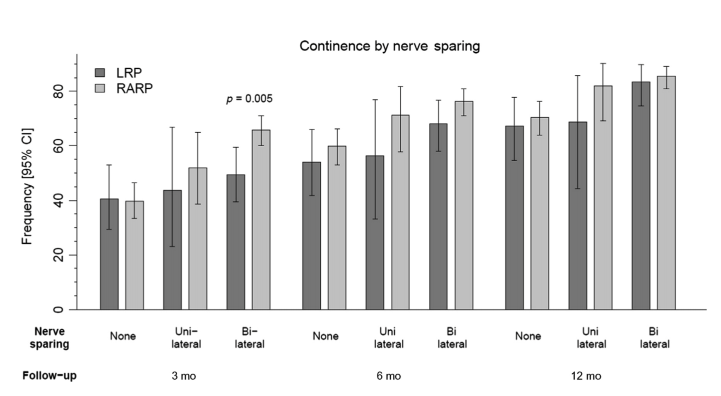
图1 随访3、6和12个月后的尿失禁情况
结果显示,在12个月时,782名患者中有701名有随访数据。术后6个月和12个月时,RARP患者的排尿情况均更好,但差异不具有统计学意义(分别为p = 0.068和0.38)。基线时有性交能力并接受神经疏通手术的患者报告说,RARP术后的性能力明显提高,其定义是在3(p = 0.005)、6(p = 0.018)和12 个月(p = 0.013)时维持足以进行性交的勃起的能力。本研究没有调查不同吻合技术的影响,这是一个局限。
综上所述,LRP和RARP都为前列腺癌患者提供了高标准的治疗。然而,机器人辅助在特定领域提供了更好的功能结果,如在适合保留神经的RP患者中的性能力和早期尿失禁方面。
原始出处:
Jens-Uwe Stolzenburg , Sigrun Holze , Vinodh-Kumar-Adithyaa Arthanareeswaran et al. Robotic-assisted Versus Laparoscopic Radical Prostatectomy: 12-month Outcomes of the Multicentre Randomised Controlled LAP-01 Trial. Eur Urol Focus. Feb 2022.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#多中心#
53
#对照#
52
#LAP#
73
#腹腔镜#
67
#机器人#
61
#根治术#
66
#机器人辅助#
71
#机器#
62
#根治#
49