JAMA:地塞米松结合卡非佐米或硼替佐米治疗多发性骨髓瘤的效果比较(ENDEAVOR研究)
2015-12-06 QQduhq 译 MedSci原创
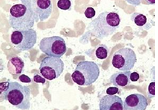
硼替佐米与地塞米松结合使用是治疗复发或难治性多发性骨髓瘤标准的治疗方案。有研究人员发现,卡非佐米与地塞米松结合使用治疗也有较好的效果。本研究的目的是比较卡非佐米和地塞米松联合与硼替佐米和地塞米松联合使用治疗复发或难治性多发性骨髓瘤患者的效果。
背景:硼替佐米与地塞米松结合使用是治疗复发或难治性多发性骨髓瘤标准的治疗方案。有研究人员发现,卡非佐米与地塞米松结合治疗也有较好的效果。本研究的目的是比较卡非佐米和地塞米松联合与硼替佐米和地塞米松联合使用治疗复发或难治性多发性骨髓瘤患者的效果。
方式:该研究为随机、三期、非盲、多中心研究,研究人员随机分配患有1-3个复发或难治性多发性骨髓瘤的患者进入2组接受治疗。1组患者接受卡非佐米结合地塞米松治疗方案(卡非佐米组),另一组患者接受硼替佐米结合地塞米松治疗方案(硼替佐米组)。并根据既往接受蛋白酶体抑制剂治疗、既往治疗效果、肿瘤的国际分期等进行分层。患者若不出现病情进展,则在第一周期的第1、2天接受卡非佐米20mg/(m2·天),之后剂量为56mg/m2,以静脉输液的形式,时长为30分钟,同时以口服或静脉输液的方式补充地塞米松20mg;硼替佐米组患者以静脉输液或皮下注射硼替佐米1.3 mg/m2和口服或静脉输液地塞米松20mg。研究观察的主要目标是患者生存率。所有患者至少接受一种药物进行治疗。
结果:2012年6月20日-2014年6月30日期间,929名患者参与了该试验,随机分配到卡非佐米组(464人)和硼替佐米组(465人)。卡非佐米组患者平均随访时长为11.9个月(IQR:9.3-16.1),而硼替佐米组患者平均随访时长为11.1个月(IQR:8.2-14.3)。卡非佐米组患者平均无肿瘤进展生存率为18.7个月(95%CI:15.6以上),硼替佐米组患者平均为9.4个月(95%CI:8.4-10.4),与实验前的分析相符(HR:0.53,95% CI:0.44-0.65];p<0.0001)。
卡非佐米组出现不良事件的的患者有18人(4%),出现严重不良事件的患者有224人(48%);而硼替佐米组出现严重不良事件的的患者有16人(3%),出现严重不良事件的患者有162人(36%)。患者最常发生的3级不良事件为贫血、高血压、血小板减少和肺炎。卡非佐米组贫血患者有67人(14%),高血压患者有41人(9%),血小板减少患者有39人(8%)肺炎患者有32人(7%);硼替佐米组贫血患者有45人(10%),高血压患者有12人(3%),血小板减少患者有43人(9%),肺炎患者有36人(8%)。
结论:对于复发或难治性多发性骨髓瘤患者,在某些情况下,地塞米松与卡非佐米可能也不失为一种较理想的治疗方案。
原始出处:
小提示:本篇威廉亚洲官网
需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言







#Endeavor#
45
#多发性#
47
好文章,值得收藏
137
好文章,值得收藏
175