Nature:研究人员发现可能有助于预防阿尔茨海默病的信号分子
2021-07-14 MedSci原创 MedSci原创
一部分星形胶质细胞试图通过释放一种叫做白细胞介素 3 (IL-3) 的分子将杀伤性小胶质细胞转化为不再消灭神经元而是专注于清除淀粉样蛋白 β 沉积物和tau 缠结。
神经胶质细胞生态系统内的通信对于神经元和大脑健康至关重要,但是神经胶质细胞对阿尔茨海默病 (AD) 患者大脑中 β-淀粉样蛋白 (Aβ) 和神经原纤维 tau 的积累和清除的影响知之甚少,尽管人们越来越意识到这些是治疗上重要的相互作用。
发表在《自然》杂志上由马萨诸塞州综合医院 (MGH) 的研究人员领导的一项研究确定了一种特殊的信号分子,该信号分子可以帮助改变炎症和免疫系统以预防阿尔茨海默病。研究发现,一部分星形胶质细胞试图通过释放一种叫做白细胞介素 3 (IL-3) 的分子将杀伤性小胶质细胞转化为不再消灭神经元而是专注于清除淀粉样蛋白 β 沉积物和tau 缠结。
当神经元开始死亡时,与阿尔茨海默病相关的认知能力下降。神经元死亡可能是由不当的免疫反应和过度的神经炎症或大脑炎症引起的,或由高水平的淀粉样蛋白 β 沉积物和 tau 缠结引发。
“一旦神经元开始大量死亡,称为小胶质细胞和星形胶质细胞的脑细胞——它们通常是清理碎片的培养细胞——就会被激活以引起神经炎症,以保护大脑。它们在进化上被编程为消灭大脑区域神经元细胞死亡过多,因为它可能是由于感染引起的,必须阻止其传播,
在阿尔茨海默病的情况下,淀粉样蛋白 β 沉积物和 tau 缠结引起的神经元细胞死亡激活了这种反应。随着神经炎症的发生,细胞死亡的数量至少是由斑块和缠结引起的死亡数量的 10 倍。所以阻止神经炎症的进展很关键!
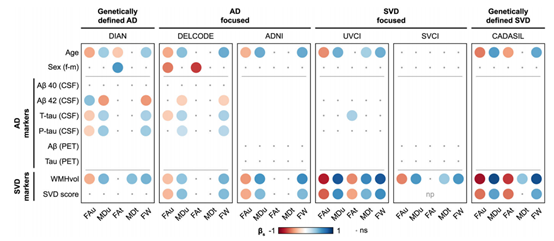
该研究结果发现,星形胶质细胞来源的白细胞介素 3 (IL-3) 编程小胶质细胞可以改善 AD 的进展。星形胶质细胞组成性地产生 IL-3,它引发小胶质细胞的转录、形态和功能编程,赋予它们急性免疫反应程序、增强的运动性以及聚集和清除 Aβ 和 tau 聚集体的能力。这些变化限制了 AD 病理和认知能力下降。研究员将 IL-3 确定为星形胶质细胞 - 小胶质细胞串扰的关键介质和 AD 治疗干预的节点。

“知道星形胶质细胞通过 IL-3 与小胶质细胞对话以教育小胶质细胞并帮助它们降低阿尔茨海默病的严重程度,这可能具有重要的临床意义,”Swirski 说。“williamhill asia 现在可以考虑一下如何使用IL-3不仅有助于遏制了神经炎症--是进行神经元细胞死亡的阿尔茨海默氏病的大头,但也诱使小胶质细胞扫清Aβ 和 tau 聚集体。
“在大脑中发现 IL-3 令人惊讶,”第一作者、系统生物学中心的讲师 Cameron McAlpine 博士说。“williamhill asia 的研究结果表明,星形胶质细胞和小胶质细胞之间通过 IL-3 的通讯是一种重要的机制,它可以通过指导小胶质细胞适应保护功能来预防阿尔茨海默病。随着进一步研究,IL-3 信号可能提供一个新的治疗机会来对抗神经系统疾病。
参考文献:Astrocytic interleukin-3 programs microglia and limits Alzheimer's disease, Nature (2021). DOI: 10.1038/s41586-021-03734-6 , www.nature.com/articles/s41586-021-03734-6
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言














#Nat#
52
#研究人员#
66
#阿尔茨#
42
#阿尔茨海默#
46
#阿尔茨海#
46