JAHA:颈动脉狭窄快速筛查又添新手段-基于视频运动分析
2022-08-18 MedSci原创 MedSci原创
使用VMA系统快速筛查CAS是一种简单、准确的筛查技术,具有较好的可行性、可接受的敏感性和特异性。
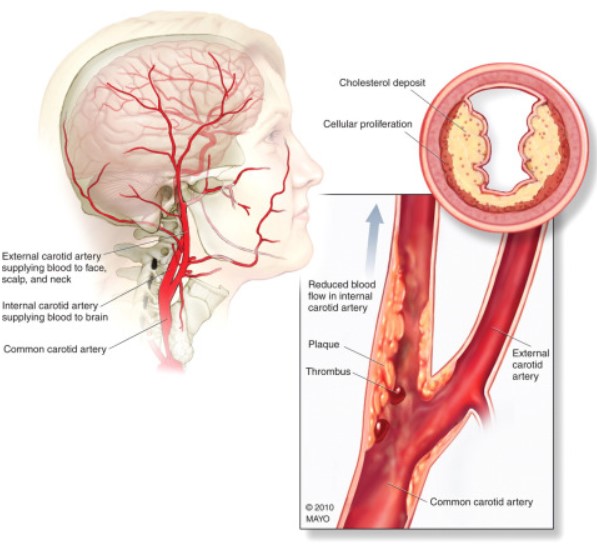
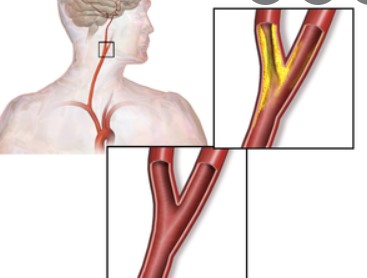
颈动脉狭窄(CAS)是缺血性脑卒中的常见病因,CAS的早期发现可改善患者的预后。颈动脉听诊虽然有效,但其在CAS筛查中的敏感性和特异性较低。目前,颈动脉多普勒超声是评估颈动脉病变严重程度首选的无创手段。然而,它受到患者肥胖、颈部不活动和观察者间变化的限制。此外,这项检查方法价格昂贵,阻碍了它在临床上的使用。
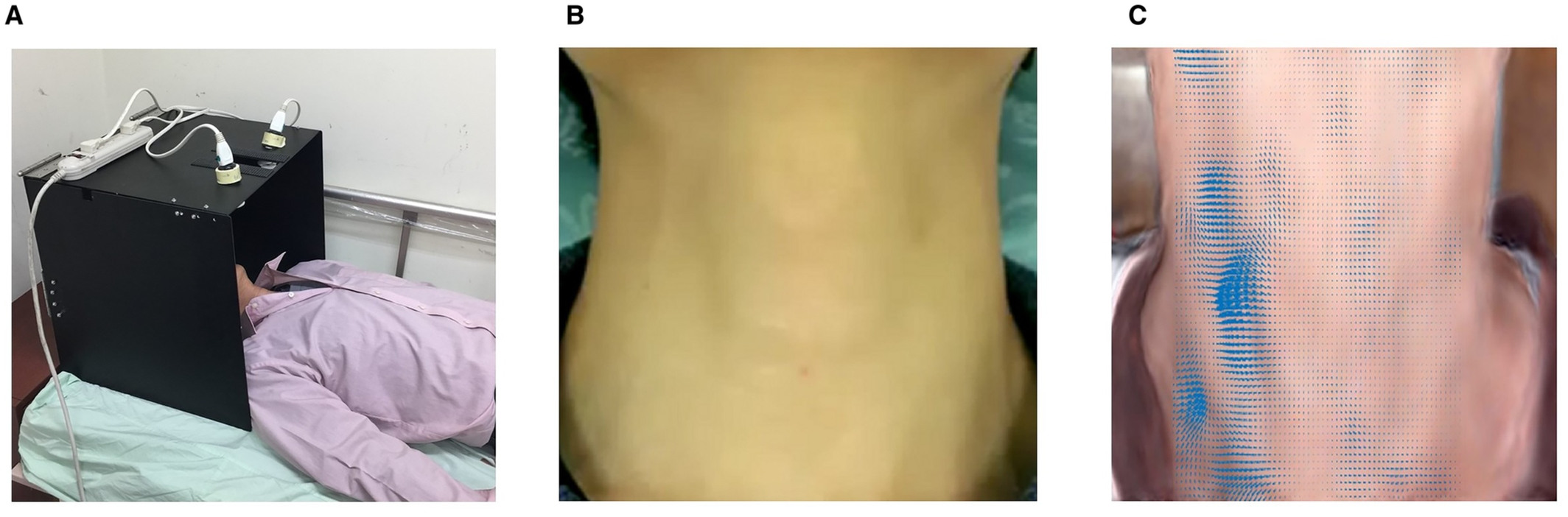
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究提出了一种新型的无创和非接触式检测技术,利用基于视频的运动分析(VMA)从皮肤表面的细微脉冲中提取有用的信息,以筛选CAS。

研究人员前瞻性地纳入了202例有颈动脉多普勒超声数据的患者。使用商业移动设备拍摄了一段短短的30秒的颈部视频片段,并通过VMA在盲法下对皮肤运动变化幅度进行数学量化分析。前40名受试者用采用VMA方案检查,并定义了临界值,后162名受试者用于验证。
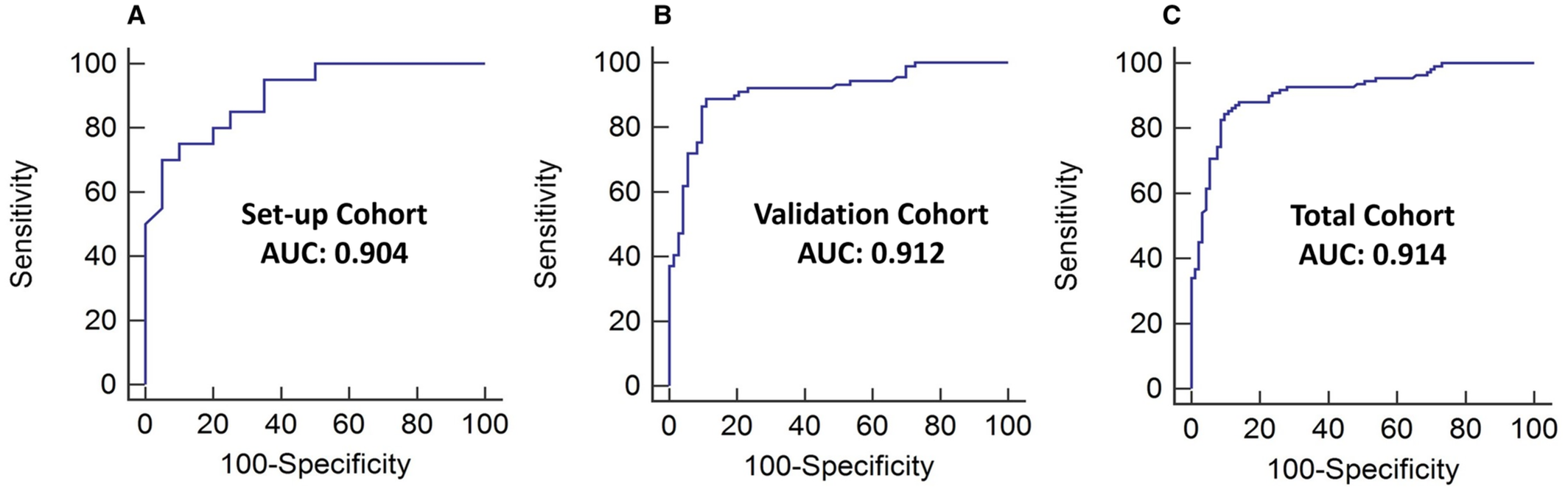
总的来说,202名受试者中有54%的受试者有超声确认的颈动脉狭窄。使用受试者工作特征曲线分析,VMA得到的差异值用于区分CAS患者和非CAS患者的曲线下面积非常好(曲线下面积为0.914[95%CI为0.874-0.954];P<0.01)。VMA得到的CAS筛查差异值的最佳临界值为5.1,灵敏度为87%,特异性为87%。诊断的准确性在不同的受试者亚组中一致高。
由此可见,使用VMA系统快速筛查CAS是一种简单、准确的筛查技术,具有较好的可行性、可接受的敏感性和特异性。
原始出处:
Cheng‐Hsuan Tsai.et al.Detection of Carotid Artery Stenosis Based on Video Motion Analysis for Fast Screening.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.122.025702
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#颈动脉#
62
#AHA#
61
#动脉狭窄#
135