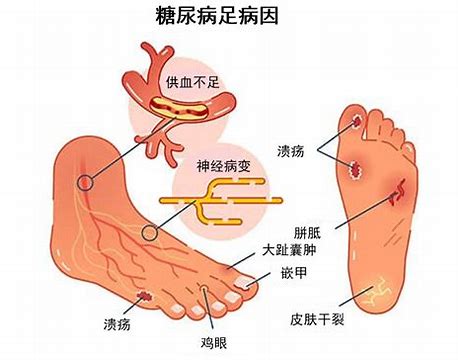
PRS:糖尿病足一定要截肢?别忘了还能选择显微外科手术保肢!
2021-03-12 MedSci原创 MedSci原创
重建显微手术是糖尿病患者下肢未愈合伤口的有效保肢选择。本文旨在分享糖尿病人群显微外科保肢的功能性步行结果和确定糖尿病足通过显微手术皮瓣移植后会截肢的危险因素。
一些显微外科医生可能会在为糖尿病肢体保肢提供皮瓣移植方面犹豫不决,因为他们担心额外的、通常是晚期的糖尿病合并症会增加皮瓣丢失和最终截肢的风险。挽救糖尿病肢体的失败的尝试并不少见。因此,了解这一患者群体中合并症的患病率及其增加皮瓣失败和最终截肢的风险的程度将更好地为手术计划提供信息。此外,了解长期结果将导致更好的风险分层和适当的医疗资源分配。

这项研究是对在2011年8月至2018年1月期间进行的下肢游离组织移植的回顾性研究。纳入标准包括是否接受自由组织移植、年龄超过18岁以及糖尿病的诊断。根据长期结果将患者分为成功保肢或截肢队列。该研究结果发布于PRS3月刊,报道了显微外科保肢的长期结果和再次截肢的危险因素,并在文章中对既往相关研究结果作总结及比较。

供体因素、伤口位置、皮瓣功能和审美偏好决定了的具体使用的皮瓣区域及类型。由于糖尿病肢体患者的吻合血管选择中通常存在钙化斑块,因此在游离组织移植手术中需特别考虑。如果近端皮瓣的流入受到严重钙化硬化的影响,研究者建议采用双端锥形微针的无创性“由内到外”技术。在这种情况下,钙化的血管应该以最小的力量处理,以限制钙化斑块的内膜破裂;又如果受体和供体血管已经钙化,可以将大隐静脉补片“端对端”地插入相关血管之间。为了避免钙化内膜破裂和血管血栓形成的风险,可以由内向外缝合补片。这些方法最大限度地减少了继发于严重钙化的内膜瓣形成和解决大小不匹配的问题。如果钙化也损害了深静脉,也可以使插入的大隐静脉补片流出到浅静脉系统。
研究中的所有患者都采用相同的术后方案。方案如下:前5天进行皮瓣检查,第7天开始悬垂检查,第7天至6个月内按压包扎。所有患者在术后前4周内均保持非负重状态。从穿步行靴开始行渐进式负重,并进行物理治疗。当需要时,会有足部矫形师定制相关鞋具。为了确保鞋具不会导致任何复发情况,研究者要求患者经常复查,并对患者进行自我监测方面的宣教。
共有64例患者符合标准。即刻皮瓣移植总成功率为94%。长期来看,50名患者(78.1%)成功保肢,14名患者(21.9%)需要大腿截肢。4例因急性皮瓣丢失需截肢,10例因延迟并发症(血肿、感染、复发不愈合)需截肢。平均截肢时间为5.6个月。截肢的危险因素是终末期肾病(OR30.7;p=0.0087)、后足创伤(OR4.6p=0.020)、血红蛋白A1C水平升高超过8.4%(OR1.4p=0.020)以及伤口感染(OR6.1p=0.003)。
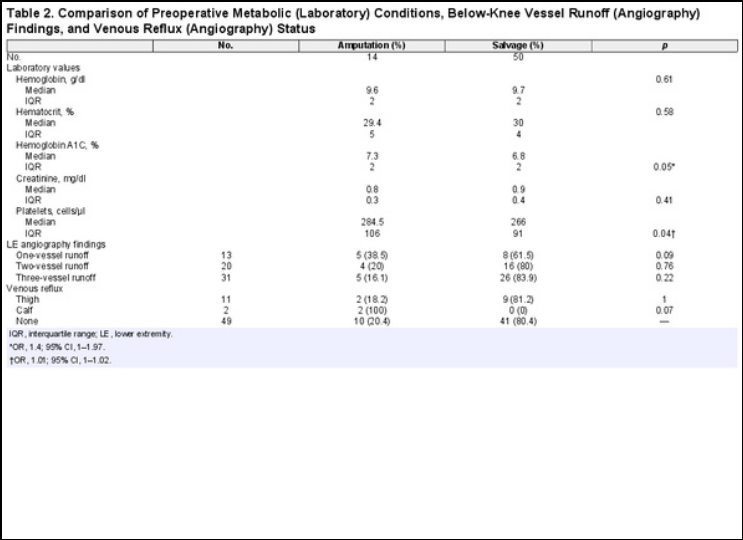
截肢患者和保肢患者的人口统计学和医疗条件相似。

需截肢的患者的基线血红蛋白A1C和血小板水平显著高于保肢患者,但下肢血管通畅率差异不显著。
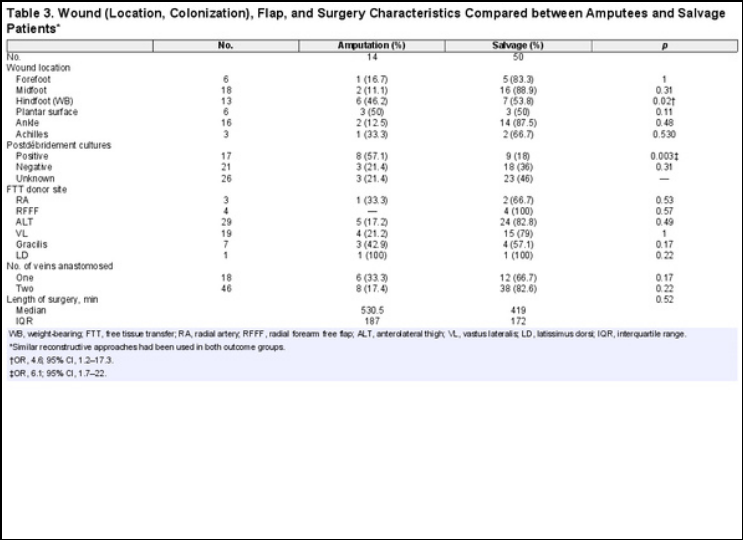
伤口位置、伤口定植和皮瓣特征如图所示。
64名患者中有4名(6%)发生了手术损伤,这些患者都是将需截肢患者:2/4(50%)发生在急性皮瓣受损后2周内,1/4(25%)发生在5个月随访时,原因是旁路移植物感染和坏疽,1/4(25%)发生在7个月随访时,原因是移植区域缺血。64名患者中有4名(6%)出现血肿。术后期间无其他并发症发生。较长期的并发症包括出现裂开和供区并发症;后两者仅影响保肢患者。

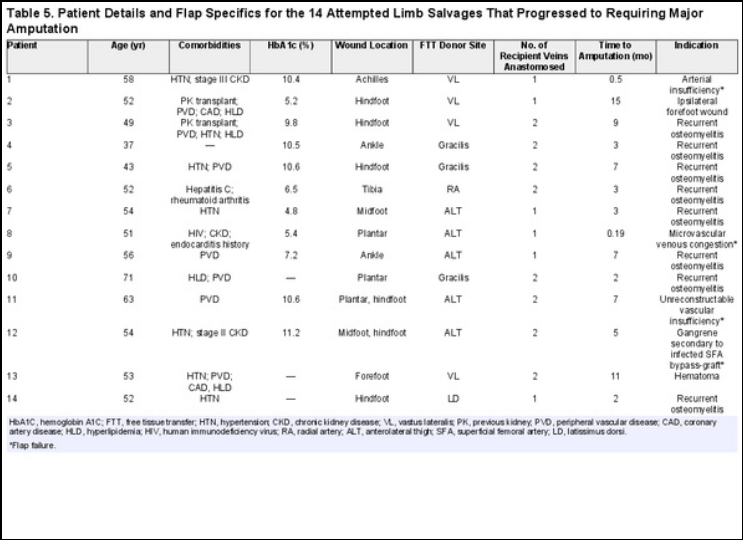
下图为截肢患者的具体信息。两名患者最终都接受了大腿截肢,在初次重建后需要第二次游离皮瓣,分别间隔了275天和875天。
在最近一次随访中,70%可以重新行走。这个亚组的总体肢体保留率为78%,总体而言,84.4%实现了行走。80%的主要截肢患者是可以步行的,相比之下,保肢患者的这一比例为85.7%(p=0.64)。在那些有活动能力的人中,58%可以独立完成,42%患者需要帮助。与截肢患者相比,保肢患者更容易独立行走。不能行走对截肢患者和成功保肢的患者有几近相同的影响。
这是第一个致力于调查糖尿病患者接受下肢游离组织移植重建后不良长期结果的危险因素的显微外科研究。游离组织移植需要广泛的围手术期资源分配,在这个效率和医疗改革的时代,了解不良结果的前兆可以加强团队努力,对保肢候选人分层,以获得理想的结果。皮瓣移植总成功率和肢体保留率分别为94%和78%。14例截肢患者中,4例因皮瓣受损而截肢,其中2例发生在术后早期。10例微血管重建成功的患者中,8例为复发性骨髓炎,1例为足部远端伤口感染,1例为血肿。截肢危险因素有终末期肾病、后足创伤、血红蛋白a1c水平升高和伤口定植。
慢性疾病的管理应该包括一个多学科的护理团队,专注于在手术前优化医疗以稳定微血管状况。根据这一点,该团队目前正在进行更高功率的多地点调查,以确认他们的结果。由于严重的内科合并症,比如终末期肾病,尚未被归类为显微外科下肢保肢手术的明确禁忌症,研究者将继续在个案的基础上考虑基于自由组织移植的肢体保肢手术。
然而,必须注意的是,部分患者会选择通过一期截肢来加速伤口愈合并恢复功能,而非游离皮瓣重建(即,不良手术候选者和患有顽固性感染、终末期肾脏疾病或尝试血运重建后血流不足的患者)。对于手术风险较高的患者,长时间全身麻醉的风险可能会大于抢救效果。尽管尝试了血运重建,但下肢血流灌注有限的患者也应考虑一期截肢。无远端灌注的血管病变肢体有顽固性清创后定植和骨髓炎的基础风险,限制了长期皮瓣的成功。
该研究的局限性在于回溯性设计和样本量小。此外,像这项研究这样的外科调查不可避免地存在一定程度的选择偏差,因为对糖尿病足治疗非常复杂,还有许多适应证的障碍。
考虑到外科医生的经验和技术熟练程度在取得良好的皮瓣效果方面的重要性,如何达到某一研究中良好的术后效果对不同的医生也是一种挑战。
越来越多糖尿病足显微外科研究反馈的积极结果,很大程度缓解了糖尿病人群中对显微吻合口开放失败的担忧。因此,在保留双足功能的同时实现伤口的最终闭合的能力使显微外科抢救成为糖尿病患者受损肢体的理想选择。
然而,由于到目前为止,对这些患者的明确治疗主要局限于血管或骨科手术的截肢,显微外科治疗尚未成为一种常规的伤口护理方式。此外,由于早期治疗通常是由药物和内分泌学驱动的,随后提供的手术治疗在很大程度上取决于转诊模式和医生个体。因此,研究者认为至关重要的是,显微外科医生应在护理过程中及早向他们的同事普及常规转诊的好处。在推动多学科糖尿病肢体护理的情况下,研究者乐观地认为,在人群基础上,可以显著改善无截肢生存率。
多处糖尿病合并症和血糖控制不良是游离皮瓣肢体保肢术后截肢的危险因素,但还是有机会成功保肢。
在整形外科中,关于糖尿病患者有无法愈合的伤口这样的情况,是通过早期安装假肢和积极的康复训练,还是采用多步骤重建或截肢的方法,哪个更好地实现闭合,这一点在整形外科中一直存在争议。考虑到这两种护理途径的财务、医疗和社会影响,准确的风险分层和患者选择至关重要。通过报道第一个致力于截肢风险评估的大型显微外科手术系列,研究者希望可以改善围手术期的决策,优化患者的生活质量。
原始文献:
Kotha Vikas S,Fan Kenneth L,Schwitzer Jonathan A et al. Amputation versus Free Flap: Long-Term Outcomes of Microsurgical Limb Salvage and Risk Factors for Amputation in the Diabetic Population.[J] .Plast Reconstr Surg, 2021, 147: 742-750.
DOI: 10.1097/PRS.0000000000007644
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













优质论文
52
#PRS#
46
学习了
84
#显微外科#
47
#外科手术#
54
#截肢#
44
谢谢MedSci提供最新的威廉亚洲官网
68
很好!!!
106
棒
98