J Clin Oncol:鲁卡帕利单药维持治疗新发卵巢癌的3期临床试验结果
2022-06-08 MedSci原创 MedSci原创
鲁卡帕利单药一线维持治疗晚期卵巢癌的疗效显著
对于一线化疗达到完全缓解(CR)或部分缓解(PR)的卵巢癌患者,维持治疗可延缓疾病复发或进展。不同分子特征的卵巢癌患者采用PARP抑制剂奥拉帕利和尼拉帕利维持治疗的效果千差万别,携带BRCA突变的卵巢癌患者可从中获得最大的无进展生存期(PFS)益处,其次是有其他同源重组缺陷(HRD)的患者。
ATHENA试验目的是评估另一种PARP抑制剂鲁卡帕利作为一线维持疗法用于广泛乳腺癌患者(包括不携带BRCA突变或其他HRD)的效果。
在该试验中,接受细胞减灭术并对一线铂类双药化疗有反应的III-IV期高级别卵巢癌患者被随机(4:1)分至鲁卡帕利组(600 mg,2/日)或安慰剂组。并根据化疗后和手术时的HRD状态、残留病灶进行分层。主要终点是无进展生存期。
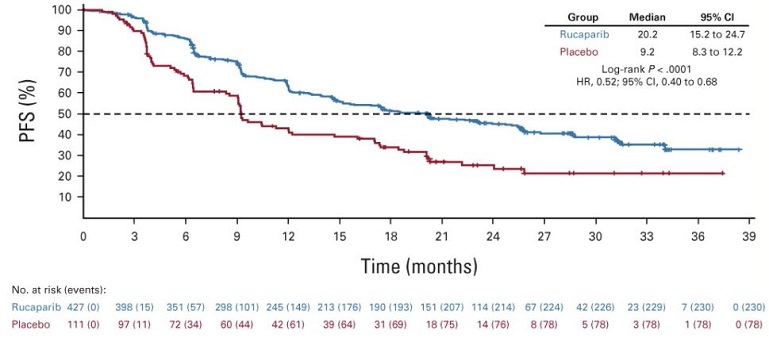
两组总患者的无进展生存率
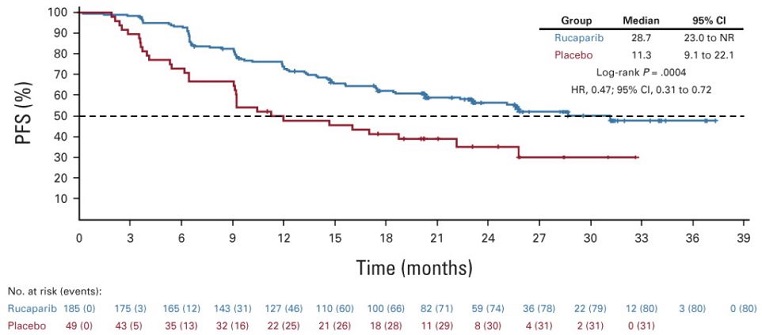
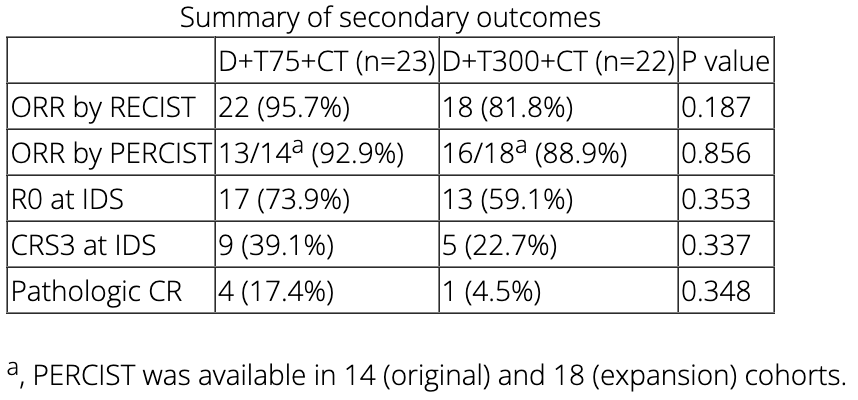
截止2022年3月23日,共有538位患者被随机分至鲁卡帕利组(n=427)或安慰剂组(n=111)(HRD患者:185 vs 49)。鲁卡帕利组和安慰剂组总患者的无进展生存期分别是20.2个月和9.2个月(风险比[HR] 0.52,p<0.0001);HRD患者的无进展生存期分别是28.7个月和11.3个月(HR 0.47,p=0.0004);HRD阴性患者的无进展生存期分别是12.1个月和9.1个月(HR 0.65)。
两组HRD阳性患者的无进展生存率
最常见的3级及以上的需紧急处理的不良反应有贫血(鲁卡帕利组 vs 安慰剂组:28.7% vs 0%)和中性粒细胞减少症(14.6% vs 0.9%)。
综上,在晚期卵巢癌患者中,无论有无同源重组修复缺陷,鲁卡帕利单药作为一线维持治疗的效果良好,与安慰剂相比可获得显著的生存益处。
原始出处:
Bradley J. Monk, et al. A Randomized, Phase III Trial to Evaluate Rucaparib Monotherapy as Maintenance Treatment in Patients With Newly Diagnosed Ovarian Cancer (ATHENA–MONO/GOG-3020/ENGOT-ov45). Journal of Clinical Oncology. June 04, 2022. https://ascopubs.org/doi/full/10.1200/JCO.22.01003
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











#3期临床#
0
#Oncol#
59
#3期临床试验#
0
学到了
85