Lancet:Tocilizumab治疗巨细胞动脉炎的有效性
2016-03-08 MedSci MedSci原创
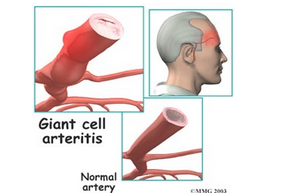
背景:巨细胞动脉炎是一种免疫介导的大中动脉疾病,常影响50岁以上人群。糖皮质激素治疗是金标准,可预防严重血管并发症,但也与大量的死亡率和发病率相关。托珠单抗(Tocilizumab),一种抗人白介素6(IL-6)受体抗体,可快速反应并缓解巨细胞动脉炎。williamhill asia 开展了首个随机临床试验研究tocilizumab在新近诊断或复发性巨细胞动脉炎患者中的安全性和有效性。方法:单中心,随机,双盲,安慰剂对照试验,
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#Lancet#
71
#mAb#
52
#动脉炎#
46
#巨细胞#
48
临床可以尝试
147
机体是一个网,
153