J Gastroenterology:肝内胆管结石是肝内胆管癌的发生风险的高危因素
2022-04-19 xuyihan MedSci原创
无症状的肝内胆管结石无法治疗,只能定期观察和随访。如果临床症状反复出现,患者应接受外科治疗。术中应尽可能清除结石,解除胆管狭窄和梗阻。
肝内胆管结石的特点是较为难治,常并发肝内胆管癌。肝内胆管癌很严重,预后很差。然而,肝内胆管癌患者肝内胆管癌的早期影像学诊断很困难,因为它很容易被结石伪影所忽视。因此,为改善肝内胆管结石患者的预后,阐明肝内胆管癌发生的预测因素至关重要。自1975年以来,日本厚生劳动省成立的肝胆管结石研究小组进行了 8 次全国的横断面调查,调查肝胆管结石的临床病理特征。本研究旨在进一步确认队列中肝内胆管癌与肝内胆管癌相关的预测因素。
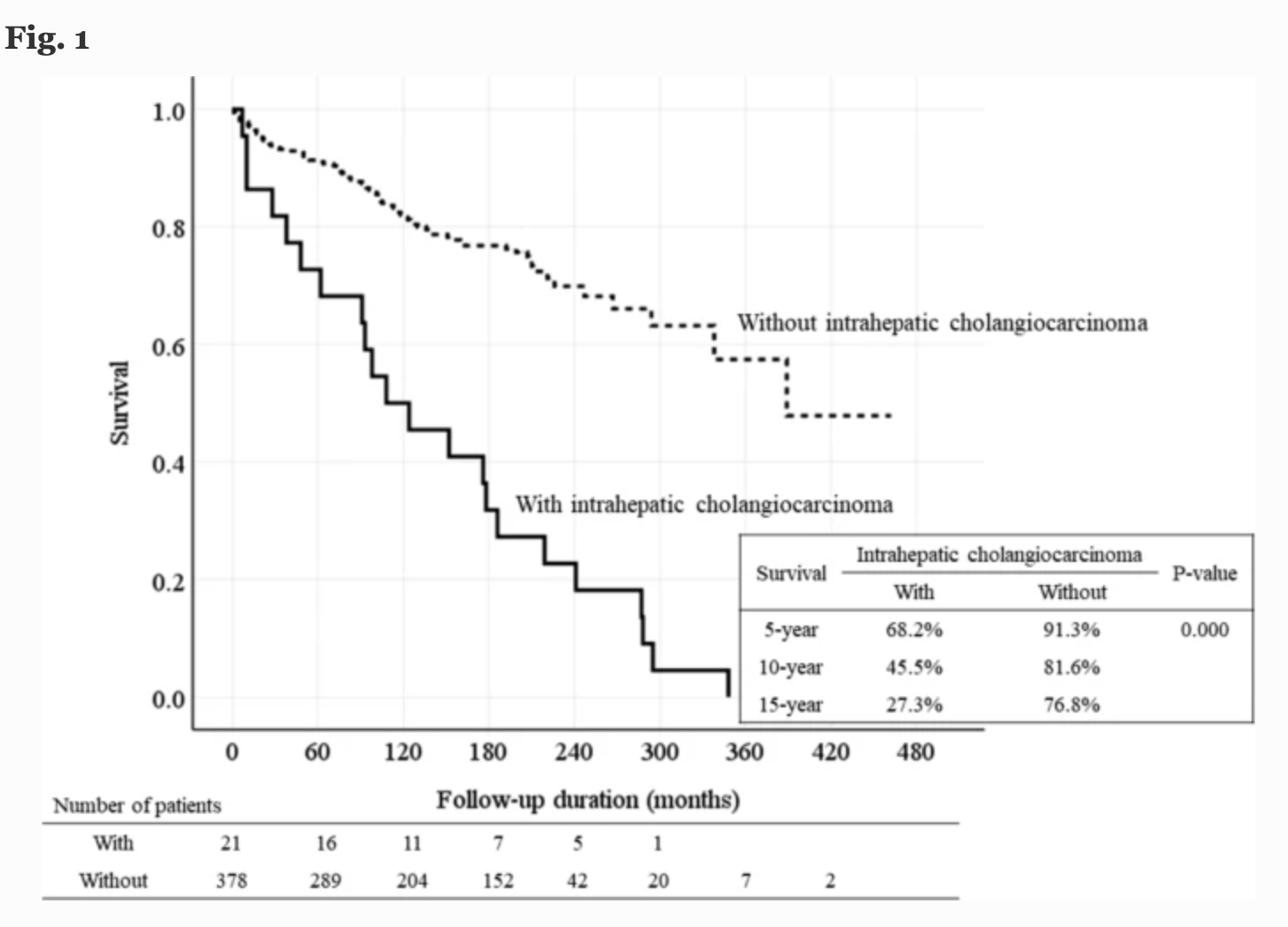
该队列由 401 名在全国肝胆管结石调查中登记的 18 年随访患者组成。在本项研究中,研究人员对既往无胆肠吻合术、发现肝萎缩、恶性肿瘤和胆道狭窄的无症状患者通过影像学研究进行定期随访观察。Cox回归分析用于阐明发展为肝内胆管癌的预测因素。
患者的中位随访期为 134 个月,其中22 名患者发展为肝内胆管癌并全部死亡。确定的独立显着因素如下:年龄 63 岁或以上(风险比 [HR] 3.344)、治疗结束时的残余结石(HR 2.445)和随访期间的胆道狭窄(HR 4.350)。三因素患者的肝内胆管癌发生率明显高于一或二因素患者。具有一个或两个预测因素的组的发病率没有差异。88.9%的胆道狭窄和肝内胆管癌患者,胆道狭窄和肝内胆管癌的诊断时间≥5年。然而,一旦发生肝内胆管癌,77。8% 的患者在 1 年内死亡。24例无症状、既往无胆肠造口术、无恶性肿瘤征象、无胆道狭窄、随访期间未接受肝内胆管结石治疗的患者中,仅有1例发生肝内胆管癌。
因此,本项研究证实在癌变方面,彻底清除结石、解除胆道狭窄可预防肝内胆管癌的发展,改善肝内胆管结石的预后。
原始出处:
Yutaka Suzuki. Et al. Predictive factors for subsequent intrahepatic cholangiocarcinoma associated with hepatolithiasis: Japanese National Cohort Study for 18 years. Journal of Gastroenterology.2022.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#Gastroenterol#
75
#GAS#
58
#AST#
62
***
66
#肝内胆管癌#
88
#Gastroenterology#
0
#胆管#
63
学习
77