ESMO Open综述:“神药”光环下的阴影?T-Dxd相关ILD/肺炎发生率超15%!
2022-08-27 MedSci原创 MedSci原创
ESMO Open:9项T-DXd单药治疗研究中药物相关间质性肺病和/或肺炎的汇总分析
Trastuzumab deruxtecan(T-DXd ,DS-8201) 是一种抗体-药物偶联物 (ADC),由抗人表皮生长因子受体 2 (HER2) 人源化单克隆抗体、四肽基可切割连接子和拓扑异构酶I抑制剂载荷组成,药物与抗体的比例很高(约8:1)。1,2该连接子在血浆中是稳定的,但可被可能在癌细胞中被上调的组织蛋白酶选择性切割。释放的有效载荷是膜通透的,允许抗肿瘤旁观者效应,半衰期短,可最大限度地减少全身暴露。
间质性肺疾病(ILD)/肺炎是多种癌症疗法(包括多种 ADC)的已知风险。 T-DXd在DESTINY系列临床试验中显示出普遍可控的安全性,其中血液学和胃肠道不良事件(AEs)是最常见的;而ILD/肺炎也被确定为值得特别关注的AE。目前, DS8201相关的ILD/肺炎的发病机制尚未完全阐明。最近一项对食蟹猴的研究表明,肺泡巨噬细胞对DS8201的摄取和再分配可能与此有关。
2019年,用于监测、评估和管理T-DXd临床试验中ILD/肺炎的研究专用威廉亚洲博彩公司 更新,包括剂量调整和支持治疗建议(表1)。与以前的威廉亚洲博彩公司 相比,该威廉亚洲博彩公司 对类固醇治疗的剂量和持续时间作出了更具体的细节介绍。经批准的DS8201标签还包括关于ILD/肺炎的警告和其管理威廉亚洲博彩公司 。
为了描述DS8201相关的ILD/肺炎,本研究对多种肿瘤类型的9项I期和II期DS8201单药治疗研究进行了汇总分析。该汇总分析包括更新威廉亚洲博彩公司 发布前后的数据,并提供了T-DXd试验中当前ILD/肺炎的诊断和管理概况。
该分析共纳入1150例患者(乳腺癌44.3%;胃癌,25.6%;肺癌,17.7%;结直肠癌,9.3%;其他癌症,3.0%)。中位治疗持续时间为5.8个月(范围:0.7-56.3个月),中位前线治疗为4线(范围:1-27)。经裁定的药物相关性ILD/肺炎的总发生率为15.4%(5级,2.2%)。大多数ILD/肺炎为低级别事件(1级或2级,77.4%);87.0%的患者是在在第一次服用DS-8201的12个月内发生第一次药物相关性ILD/肺炎事件(中位数:5.4个月;范围:<0.1-46.8)。根据数据回顾,对于53.2%的病例,判定的ILD/肺炎发病早于研究者确定的发病时间(发病时间的中位数差异:43天;范围:1-499天)。Cox回归确定了几个可能与药物相关的ILD/肺炎风险增加相关的基线因素:年龄<65岁,在日本的入组,T-DXd剂量>6.4 mg/kg,氧饱和度<95%,中度/重度肾功能损害,存在肺部合并症,首次诊断以来时间>4年。
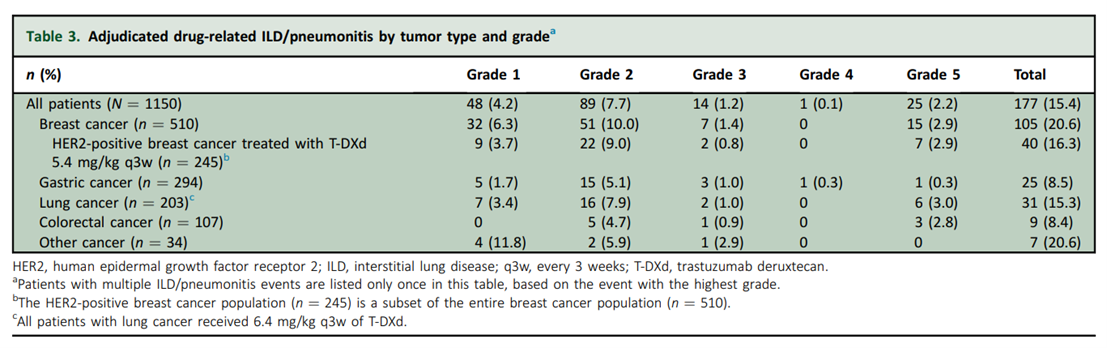
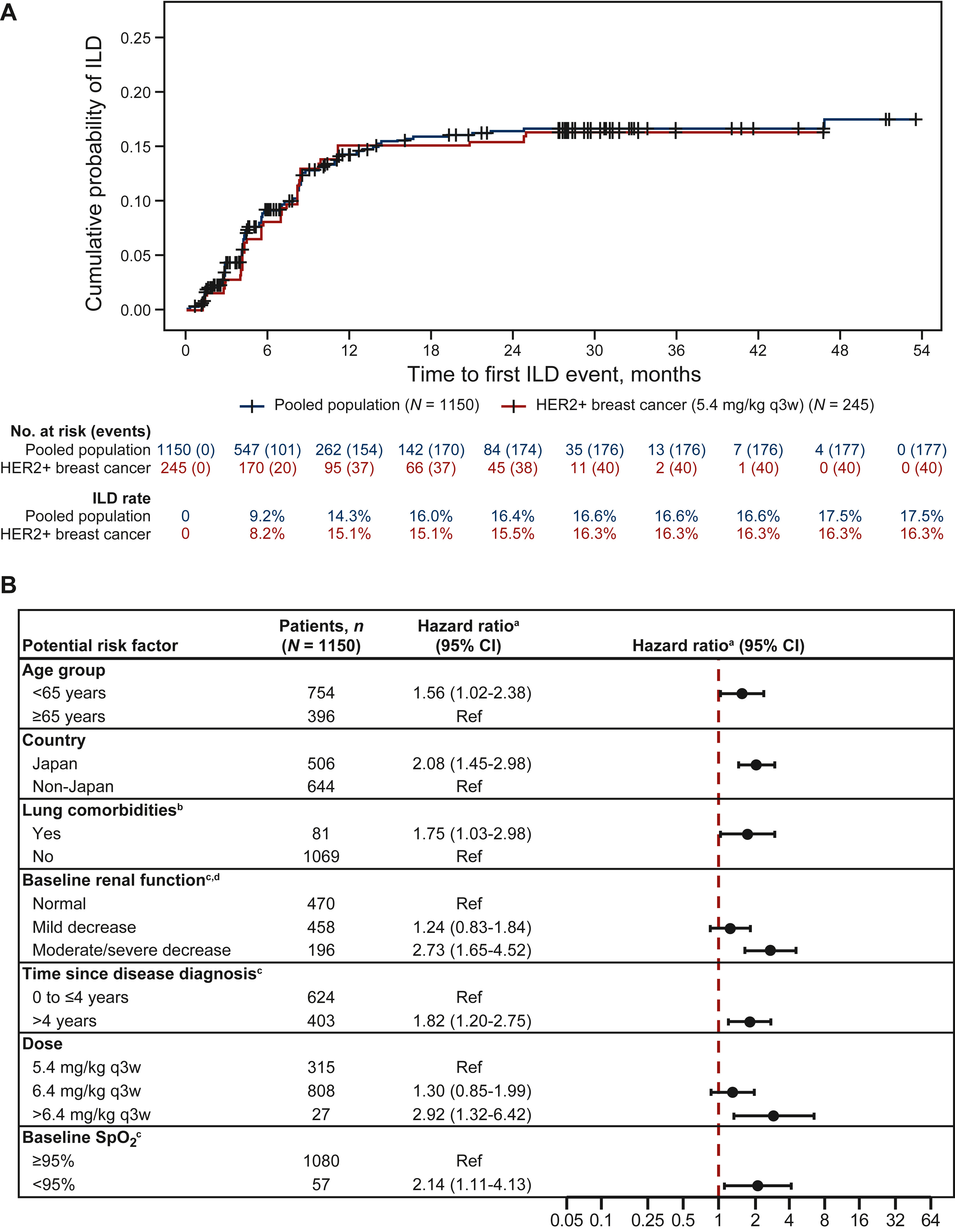
在这项对接受大量治疗的患者进行的汇总分析中,ILD/肺炎的发病率为 15.4%,大多数是低级别的,发生在治疗的前 12 个月。T-DXd治疗的获益-风险是正向的;然而,一些患者发生 ILD/肺炎的风险可能增加,需要进一步检查以确认 ILD/肺炎的危险因素。有必要对所有患者进行对ILD/肺炎的密切监测和主动管理。
原文来源:
C.A. Powell, S. Modi, H. Iwata, S. Takahashi, E.F. Smit, S. Siena, D.-Y. Chang, E. Macpherson, A. Qin, J. Singh, C. Taitt, N. Shire, D. Ross Camidge,Pooled analysis of drug-related interstitial lung disease and/or pneumonitis in nine trastuzumab deruxtecan monotherapy studies☆, ESMO Open,Volume 7, Issue 4,2022,100554,ISSN 2059-7029,https://doi.org/10.1016/j.esmoop.2022.100554.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#SMO#
62
#ILD#
60
#发生率#
75
#PE#
57
#ESMO#
89