Eur Urol Focus:勃起功能障碍患者对他达拉非的偏好超过了西地那非
2021-06-06 AlexYang MedSci原创
勃起功能障碍(ED)是一种多层面的、广泛存在于男性中的性功能障碍。血管、心理和未知的其他因素均与这种疾病有关。治疗方法包括生活方式干预、使用磷酸二酯酶-5(PDE5)抑制剂的药物治疗、真空勃起装置、注
勃起功能障碍(ED)是一种多层面的、广泛存在于男性中的性功能障碍。血管、心理和未知的其他因素均与这种疾病有关。治疗方法包括生活方式干预、使用磷酸二酯酶-5(PDE5)抑制剂的药物治疗、真空勃起装置、注射和手术干预。ED与代谢和心血管疾病有关,发病率随年龄增长而增加,同时也是心血管疾病的风险因素。

勃起功能障碍(ED)是世界范围内的一个主要问题。塔达拉非和西地那非是用于治疗ED的两种最常用的磷酸二酯酶-5抑制剂(PDE5is)。近期,有研究人员评估了一个大型线上处方平台(OPP)的患者数据,特别是分析了患者对他达拉非与西地那非的偏好性情况。
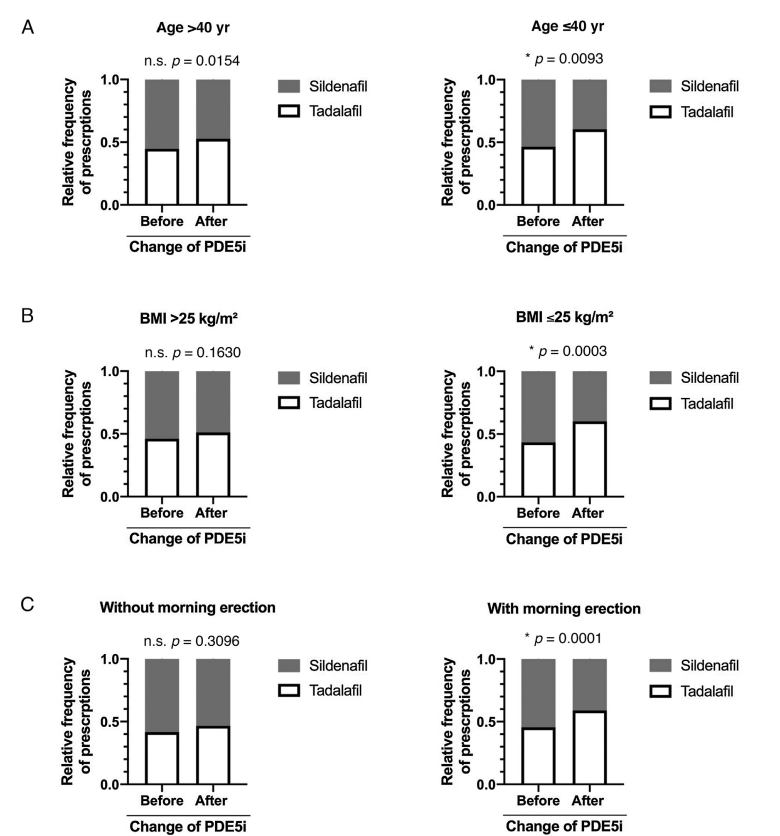
研究人员对前瞻性收集的德国OPP数据进行了回顾性分析。该数据集包括有一种或两种药物服用史的患者(n=26821)。ED患者的基线特征来自2019年5月至2020年5月期间PDE5i处方的医疗调查表。结果发现,使用两种PDE5is患者的基线特征具有可比性,中位年龄为49岁(西地那非[四分位数范围{IQR}38-57];他达拉非[IQR 39-56]),中位身体质量指数(BMI)为26 kg/m2(西地那非[IQR 24.54-29.03];他达拉非[IQR 24.49-28.69]),ED发病时间大于12个月(西地那非[87%];他达拉非[88%]),存在晨勃(西地那非[62%];他达拉非[61%])。在已经尝试过两种药物的患者中,他达拉非的处方量从30%(首单)明显增加到80%(末单)。最后,研究人员指出,年龄≤40岁、BMI≤25 kg/m2、晨间持续勃起的患者更喜欢他达拉非而不是西地那非。
ED患者对他达拉非的偏好超过了西地那非
综上所述,他们使用OPP的数据库信息,展示了尝试过两种PDE5is的患者对他达拉非的偏好,且这种偏好在年龄≤40岁、BMI≤25 kg/m2和持续晨勃的患者中尤为明显。因此,一个管理良好的OPP可用于研究更优质的健康服务。
原始出处:
Moritz von Büren, Severin Rodler, Isabell Wiesenhütter et al. Digital Real-world Data Suggest Patient Preference for Tadalafil over Sildenafil in Patients with Erectile Dysfunction. Eur Urol Focus. May 2021
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#勃起#
60
对我很有启发……
71
#功能障碍#
52
#他达拉非#
54
#勃起功能#
60
还有这研究
86