Injury:儿童和成人脾外伤后行血管栓塞术后可保留脾功能
2015-11-23 MedSci MedSci原创
荷兰阿姆斯特丹VU大学医学中心创伤外科A.G. Schimmer和同事研究儿童和成人脾外伤后行血管栓塞术后的脾功能。研究结果2015年11月19日在Injury在线发表。
荷兰阿姆斯特丹VU大学医学中心创伤外科A.G. Schimmer和同事研究儿童和成人脾外伤后行血管栓塞术后的脾功能。研究结果2015年11月19日在Injury在线发表。
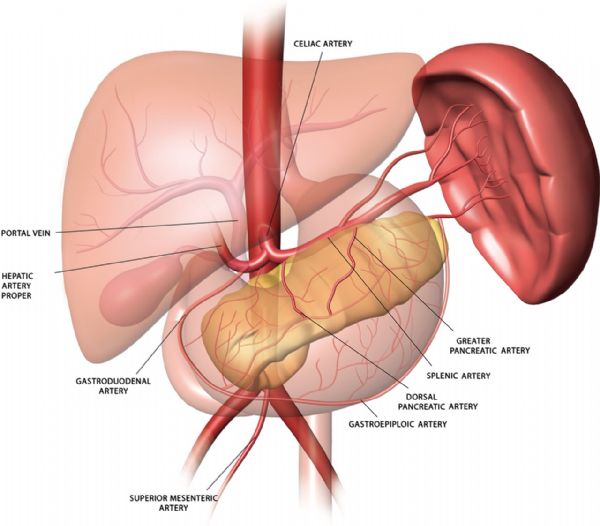
目的:近端或远端SAE(Splenic artery embolization,脾动脉栓塞)已成为外伤性脾破裂的治疗标准。理论上脾脏的免疫功能可能被保留下来,但是否真的如此还没有得到证实。因此需要开发一个可以测量剩余的脾功能的方法,用来判断脾破裂患者行SAE术后是否应该接种疫苗和/或预防性使用抗生素来预防OPSI(overwhelming post-splenectomy infection,脾切除术后爆发性感染)。
方法:2015年7月搜索Medline和Embase数据库,系统回顾文献。纳入描述至少两个外伤患者和以脾功能为主题的文献。纳入文献的标准不包括文献是否描述了SAE的过程和/或SAE的成功率。两个研究人员独立评阅文献是否符合纳入标准以及文献的质量,并提取数据。
结果:这项系统评价共纳入12个研究,其中11项研究成年患者,1项研究儿童患者。所有研究使用多种参数评估脾功能。所有研究都没有报告脾栓塞后患者发生OPSI。有11项研究发现成人和儿童脾破裂患者SAE后脾功能可以保留。
结论:除了1项研究以外,其他11项关于SAE长期效应的研究表明脾功能可以保留。然而仍然不存在一个可用的单一的参数或检测项目可以毫不含糊地表明如何判断脾破裂患者行SAE术后是否应该接种疫苗和/或预防性使用抗生素来预防OPSI。
原始出处:
A G Schimmera, AF W van der Steegb, W P Zuidemaa,et all. Splenic function after angioembolization for splenic trauma in children and adults: a systematic review. Injury. Available online 19 November 2015.
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言







学习啦,,,
88
谢谢分享,,,
94
很不错的文章,,
75
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
89
继续学习
80
继续关注
44
#Injury#
60
#血管栓塞#
53
好东西,值得分享,学习了!
143
赞
90