BMJ:俯卧位通气对Covid-19非重症低氧血症患者的影响
2022-03-30 zhangfan MedSci原创
因新冠肺炎住院的非重症低氧血症患者,俯卧位通气对改善患者住院死亡、机械通气或呼吸衰竭恶化的效果不明显

截至2021年12月,全球已有500多万人死于新冠肺炎,其中老年人、基础共病和重症是新冠肺炎死亡的重要因素。多数新冠肺炎死亡患者存在低氧血症,严重低氧血症需接受ICU机械通气,而一般低氧血症患者则进行氧气补充,大约20%的一般低氧血症患者会进展为呼吸衰竭。由于多种生理原因,俯卧位通气可以改善氧合,减少心脏和胃肠道器官导致的肺阻力,改善肺扩张,减少通气和灌注不匹配。自20世纪70年代以来,俯卧位一直是临床实践的一部分,被认为是严重急性呼吸窘迫综合征患者的标准护理手段之一。近日研究人员评估俯卧位通气对降低因Covid-19住院的非危重症患者死亡或呼吸衰竭风险的效果。
本次研究在美国及加拿大15个医院开展,实验室确诊的新冠肺炎患者参与,患者需要补充氧气并且能够通过口头指导独立进行俯卧通气,患者随机分为俯卧位组(即指导患者在睡觉时腹部俯卧)或标准护理。研究的主要终点为住院死亡、机械通气或呼吸衰竭恶化,次要结果为氧饱和度与吸入氧分数比值。
248名患者参与研究,平均年龄56岁,女性89例(36%),222例(90%)患者在随机分组时接受氧气补充。入院后前72小时,俯卧位组患者总共接受了平均6小时俯卧位通气,对照组0小时。组间主要事件风险差异不显著(俯卧位 vs 对照组:18 vs 17例,14% vs 14%,OR=0.92)。与对照组相比,俯卧位组72小时氧饱和度与吸入氧分数比值变化不显著。
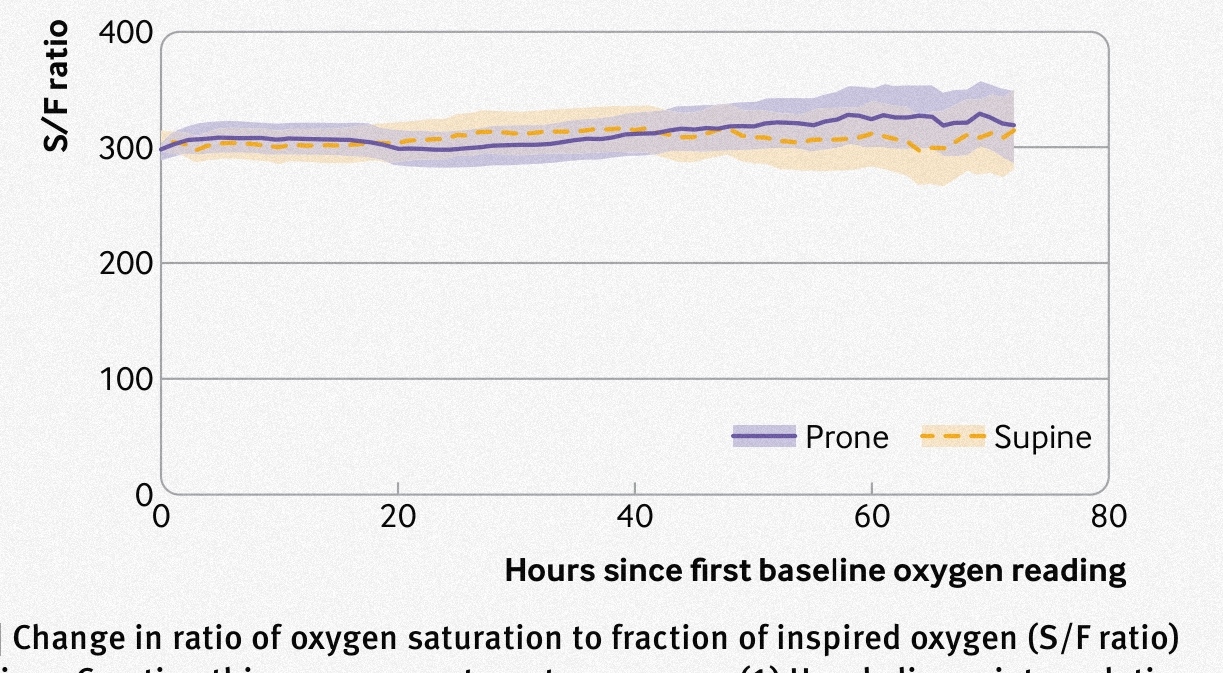
组间72小时氧饱和度与吸入氧分数比值
研究发现,对于因新冠肺炎住院的非重症低氧血症患者,俯卧位通气对改善患者住院死亡、机械通气或呼吸衰竭恶化的效果不明显,但患者俯卧位依从性差异可能是效果不显著的重要因素。
原始出处:
Michael Fralick et al. Prone positioning of patients with moderate hypoxaemia due to covid-19: multicentre pragmatic randomised trial (COVID-PRONE). BMJ,23 March,2022.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#BMJ#
52
#低氧血症#
57
#俯卧位#
53
学习
59
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
58