Movement disorders:血管周间隙和帕金森病 关系密切
2022-11-25 Freeman MedSci原创 发表于广东省
小的BG-PVS与日常生活中的运动和非运动方面的经验有关
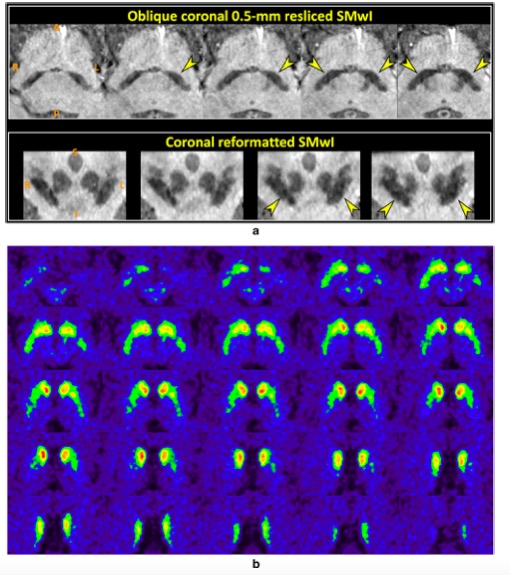
血管周围空间(PVS)是大脑血管周围充满液体的空间,是大脑液体和淋巴废物清除系统的重要通道。在神经退行性疾病患者和研究淀粉样蛋白清除的小鼠模型中,有临床和前临床证据表明,磁共振成像(MRI)上可见的PVS是脑小血管疾病和糖液清除功能障碍的标志。

图1: 论文封面图
除了MRI可见的PVS外,其他成熟的基于神经影像学的脑小血管疾病的标志物包括脑室周围和深部白质增生(WMHs)。
在帕金森病(PD)中,基底神经节区域的PVS负担(BG-PVS)已被认为是运动障碍和认知衰退进展的潜在指标。然而,有关认知方面的研究结果不一,有些研究报告说与PVS视觉负担得分没有明显的相关性。不幸的是,这些研究中有许多是用定性的视觉评分量表来评估BG-PVS的,而这种量表更容易受到评分者偏差以及上限和下限效应的影响。
有趣的是,两项基于人群的大型研究表明,大的(直径>3毫米)与小的(直径≤3毫米)PVS之间存在着病理生理上的差异,尽管在PD中没有具体证明。北曼哈顿研究的结果表明,小PVS的高负担与未来血管事件的风险增加有关,而AGES-Reykjavik研究显示,大PVS与信息处理速度下降和痴呆风险增加有关。
藉此,多伦多大学的Joel Ramirez等人, 在一个多中心的PD患者队列中,探究大型和小型BG-PVS的定量测量、全局认知和运动/非运动特征之间的关联。
他们考察了安大略省神经退行性疾病研究计划中登记的133名帕金森病患者的大、小BG-PVS与运动障碍协会统一帕金森病评定量表(MDS-UPDRS)I-IV部分和认知(蒙特利尔认知评估)之间的关联。
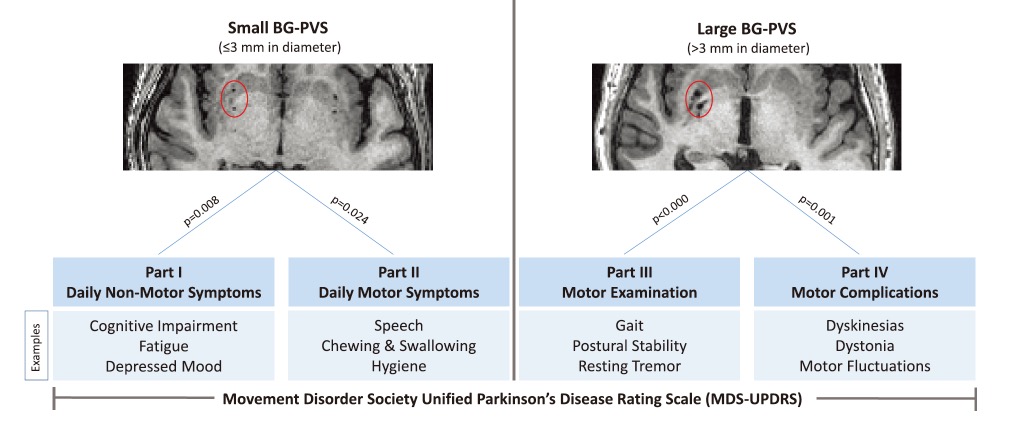
图2:论文结果图
他们发现:小BG-PVS的PD患者与MDS-UPDRS第一部分(P = 0.008)和第二部分(均P = 0.02)有关联,而大BG-PVS的患者与MDS-UPDRS第三部分(P < 0.0001)和第四部分(P < 0.001)有关联。
BG-PVS与认知能力不相关。
该研究的重要意义在于发现了:小的BG-PVS与日常生活中的运动和非运动方面的经验有关,而大的BG-PVS则与运动症状和运动并发症有关。
原文出处:
Ramirez J, Berberian SA, Breen DP, et al. Small and Large Magnetic Resonance Imaging–Visible Perivascular Spaces in the Basal Ganglia of Parkinson’s Disease Patients. _Movement Disorders_. Published online April 11, 2022:mds.29010. doi:[10.1002/mds.29010](https://doi.org/10.1002/mds.29010)
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言

















#ERS#
121
#Disord#
109
#disorders#
94
#disorder#
86
#Dis#
61