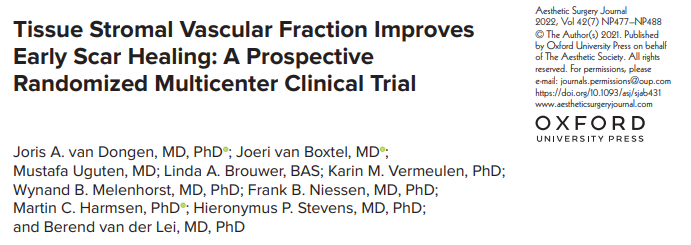
Aesthet Surg J:注射TSVF可促进早期伤口愈合,减少疤痕形成
2022-07-03 MedSci原创 MedSci原创
伤口愈合和疤痕形成取决于多种因素。鉴于异常疤痕形成的影响,旨在改善疤痕形成的干预措施将是最有利的。脂肪组织的组织基质血管部分(TSVF)是由嵌入细胞外基质的细胞的异质混合物组成。
伤口愈合和疤痕形成取决于多种因素。鉴于异常疤痕形成的影响,旨在改善疤痕形成的干预措施将是最有利的。脂肪组织的组织基质血管部分(TSVF)是由嵌入细胞外基质的细胞的异质混合物组成,含有参与伤口愈合过程的生长因子和细胞因子,例如,实质增殖、炎症、血管生成和基质重塑。近日,发表于Aesthet Surg J的一项前瞻性、双盲、安慰剂对照的随机试验旨在验证TSVF减少手术后疤痕形成的假设。
研究于2016年至2020年进行,纳入了 40 名乳房整形术患者,并随访1年。在乳房整形手术结束后,所有患者在1个乳房的水平疤痕的侧面 5cm处接受 tSVF,并在对侧乳房注射安慰剂,作为患者内部对照。主要结果是通过患者和观察者疤痕评估量表(POSAS)衡量疤痕质量。次要结果是通过照片评估和疤痕组织样本的组织学分析获得。
结果,40 名患者中有 34 名完成了随访。术后 6 个月时,根据 POSAS 问卷调查,注射 TSVF 明显改善了术后疤痕的外观。术后12个月时,没有观察到差异。根据对两组术后疤痕的照片和组织学分析的评估,注射 TSV F并未改善瘢痕。
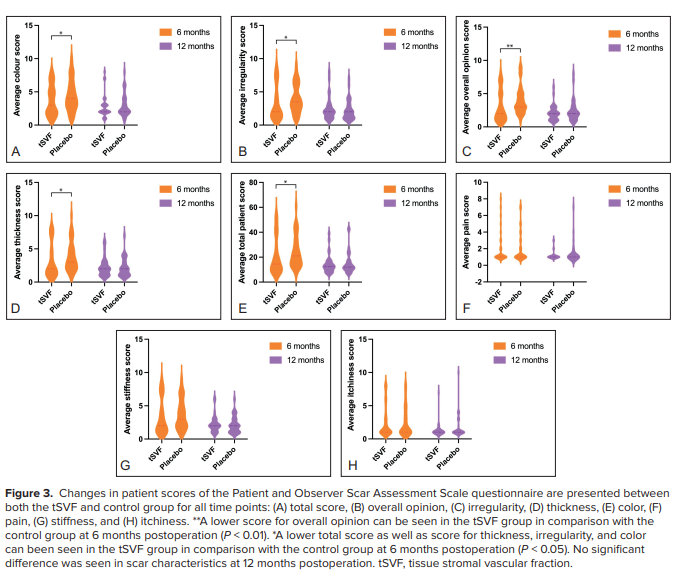
综上所述,该研究结果表明,注射 TSVF 可改善伤口愈合,减少术后6个月的疤痕形成,但在 12 个月时没有看到任何明显的优势效果。这些结果表明,TSVF 可能只是早期伤口愈合和疤痕形成的一个加速器。未来的研究应关注这些早期过程,以阐明 TSVF 发挥其作用的具体机制。
原始出处:
Joris A van Dongen, et al., Tissue Stromal Vascular Fraction Improves Early Scar Healing: A Prospective Randomized Multicenter Clinical Trial. Aesthet Surg J. 2022 Jun 20;42(7):NP477-NP488. doi: 10.1093/asj/sjab431.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#EST#
60
学习了
60
认真学习~
0
#伤口愈合#
85
#疤痕#
87