Pancreatology:早期细菌感染是证实感染性胰腺坏死患者死亡率增加的独立危险因素
2022-01-09 MedSci原创 MedSci原创
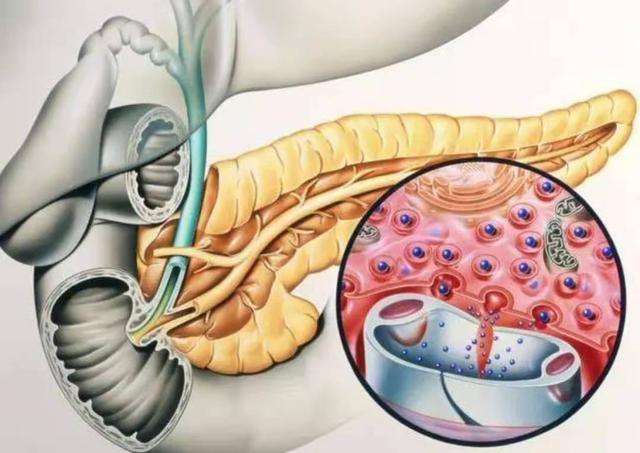
胰腺炎是胰腺因胰蛋白酶的自身消化作用而引起的疾病。胰腺有水肿、充血,或出血、坏死。
感染性胰腺坏死(IPN)是急性胰腺炎(AP)最严重的并发症之一,是导致该病死亡的主要原因之一。尽管在治疗方面取得了重大进展,但AP相关的死亡率仍然高达15至20%。最早的观察表明,在急性坏死性胰腺炎中,死亡率随时间变化的性质是动态的。推迟开放手术可以提高生存率。IPN的早期诊断与早期干预是一致的,因为感染的存在会引发治疗的提前干预。有限的数据表明,早期感染与IPN不良的临床结果相关。本研究的目的是要确定死亡率与早期IPN发展之间的关系。
 为此,研究人员对纳入的IPN患者进行了国际多中心回顾性队列研究,通过胰腺(周围)收集物的阳性微生物培养对是否存在感染进行证实。使用Cox 回归分析评估感染发作时间、干预时间和死亡率之间的关联。
为此,研究人员对纳入的IPN患者进行了国际多中心回顾性队列研究,通过胰腺(周围)收集物的阳性微生物培养对是否存在感染进行证实。使用Cox 回归分析评估感染发作时间、干预时间和死亡率之间的关联。
研究人员评估了 2000 年至 2016 年来自 3 大洲 19 个医疗中心的 743 名细菌培养证实存在感染的 IPN 的患者,所有患者的疾病死亡率为 20.9% (155/734)。早期感染与较高的死亡率相关,早期感染发生一般发生在急性胰腺炎出现后的前 4 周内。在调整合并症、高龄、器官衰竭、肠内营养和肠外营养后,早期感染(≤4 周)和早期开放手术(≤4 周)与死亡率增加相关 [HR: 2.45 (95% CI: 1.63-3.67) ), p < 0.001和HR: 4.88 (95% CI: 1.70–13.98), p = 0.003]。晚期开放手术、早期或晚期微创手术、早期或晚期经皮引流与死亡率之间没有关联(p > 0.05)。
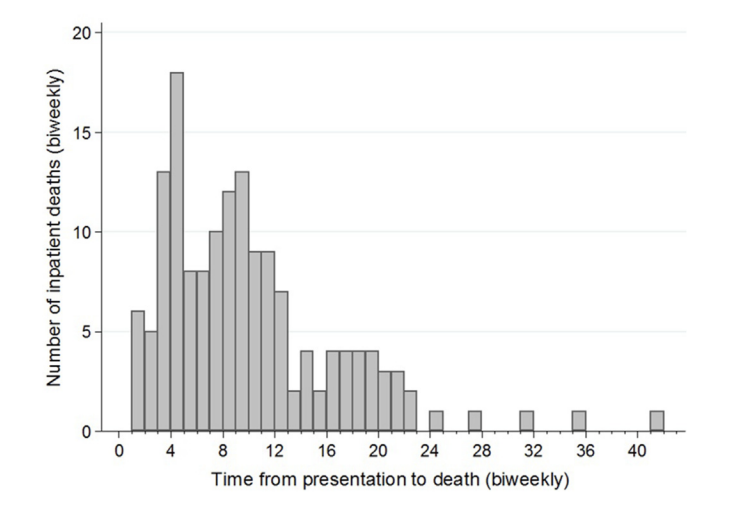
图:坏死性胰腺炎随时间变化的死亡率
本项研究证实IPN患者早期感染与死亡率增加有关,与干预无关。早期手术仍然是死亡率过高的一个强有力的预测因素。
原始出处:
Robert A.Moran. Et al. Early infection is an independent risk factor for increased mortality in patients with culture-confirmed infected pancreatic necrosis. Pancreatology.2022.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#感染性#
60
#患者死亡#
65
#独立危险因素#
66
#细菌感染#
60
#坏死#
69
#CRE#
58