Ther Adv Med Oncol:中肿石明教授团队回顾性研究发现仑伐替尼+特瑞普利单抗+肝动脉灌注化疗(HAIC)可改善晚期肝细胞癌患者预后
2021-12-29 yd2015 MedSci原创
研究表明,与lenvatinib单独治疗相比,LeToHAIC组(Lenvatinib + toripalimab +HAIC)可改善晚期肝细胞癌患者的预后,并且毒性可耐受。
Lenvatinib(仑伐替尼)是晚期肝细胞癌(HCC)的一线治疗药物,但预后仍不理想。近年来,肝动脉灌注化疗(HAIC)和免疫检查点抑制剂(ICIs)对晚期肝细胞癌显示出良好的治疗效果。考虑到不同的抗恶性肿瘤机制,结合这三种治疗可能改善结果。因此,来自中山大学肿瘤防治中心的石明教授团队开展了相关研究,旨在比较lenvatinib(仑伐替尼)、toripalimab(特瑞普利单抗)+ HAIC对比lenvatinib单药治疗晚期肝细胞癌的疗效和安全性。相关结果发表在Therapeutic Advances in Medical Oncology杂志上。

这是一项回顾性研究,包括患者lenvatinib[8mg(≤60kg)或12mg (>60kg) qd)或lenvatinib toripalimab + HAIC [LeToHAIC组,在HAIC前0-1周使用lenvatinib,每次HAIC周期前0-1天使用toripalimab 240mg,和HAIC FOLFOX方案。比较两组的无进展生存期(PFS)、总生存期(OS)、客观缓解率(ORR)和治疗相关不良事件。
在2019年2月24日-2019年8月2日期间,157例患者符合纳入本研究的标准:71例患者接受了lenvatinib、toripalimab + HAIC三联疗法(LeToHAIC),86例患者接受了lenvatinib单药治疗。LeToHAIC组的中位PFS为11.1个月[95%CI, 7.85 14.35],而lenvatinib组的中位PFS为5.1个月[HR= 0.48;95%CI, 0.33 0.7;p<0.001]。LeToHAIC组的中位OS未达到,而lenvatinib组的中位OS为11个月(95% CI, 8.14 13.86) [HR = 0.4;95%CI, 0.24 0.66;p<0.001)。
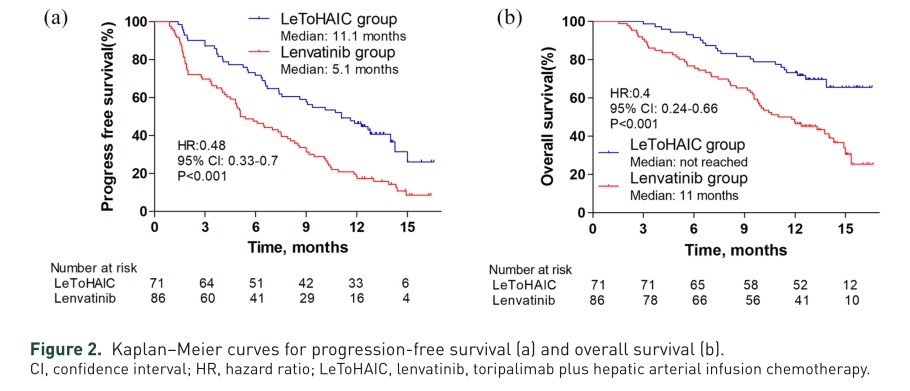
两治疗组的PFS和OS差异
亚组分析,无肝外转移患者中,LeToHAIC组中位PFS较lenvatinib单药组延长,分别为11.63 (95% CI, 8.88–14.38)和7.5(95% CI, 5.35–9.65) 个月(p = 0.004);同样,LeToHAIC组中位OS较lenvatinib单药组延长,分别为未达到和13.77 (95% CI, 11.35–16.19)个月(p = 0.001)。
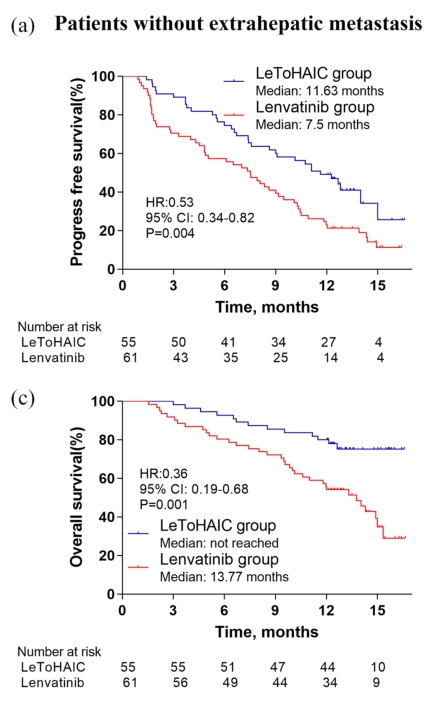
无肝外转移患者两治疗组的PFS和OS差异
而在伴有肝外转移患者中,LeToHAIC组中位PFS较lenvatinib单药组延长,分别为6.6(95% CI, 0.66–12.55) 和4.17 (95% CI,2.21–6.13)个月(p = 0.009);同样,LeToHAIC组中位OS较lenvatinib单药组有延长趋势,分别为11.37 (95% CI, 6.79–15.94)和8.17 (95%CI, 4.69–11.65) 个月(p = 0.09)。

伴有肝外转移患者两治疗组的PFS和OS差异
基于RECIST标准,LeToHAIC组的DCR和ORR显著高于lenvatinib组(90.1% vs 72.1%, p = 0.005; 59.2% vs 9.3%,p<0.001)。基于mRECIST标准,LeToHAIC组的DCR和ORR也显著高于lenvatinib组(90.1% vs 72.1%,p = 0.005;67.6% vs 16.3%,p<0.001)。此外,根据修改后的RECIST标准,LeToHAIC组中14.1%和21.1%的患者获得了所有病灶的完全缓解和肝内靶病灶的完全缓解。
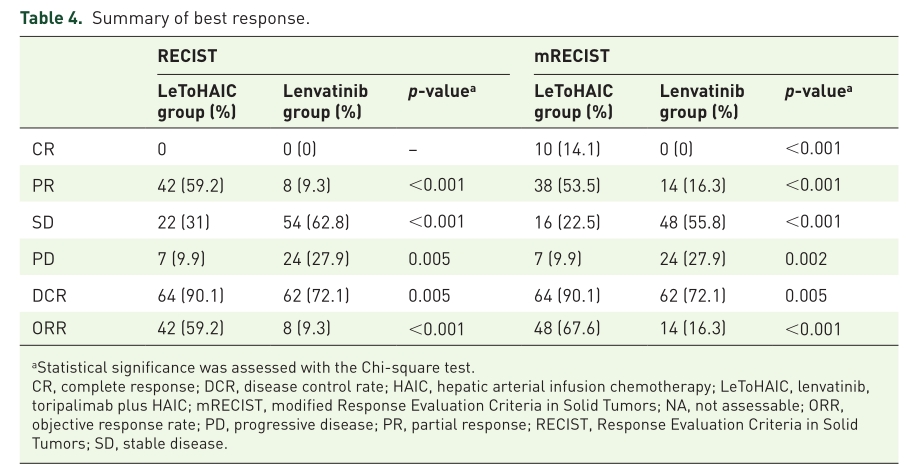
不同标准的疗效评估
LeToHAIC组3/4级治疗相关不良事件发生率高于lenvatinib组,包括中性粒细胞减少(8.5% vs 1.2%)、血小板减少(5.6% vs 0)和恶心(5.6% vs 0)。
综上,研究表明,与lenvatinib单独治疗相比,LeToHAIC组(Lenvatinib + toripalimab +HAIC)可改善晚期肝细胞癌患者的预后,并且毒性可耐受。
原始出处:
He MK, Liang RB, Zhao Y, Xu YJ, Chen HW, Zhou YM, Lai ZC, Xu L, Wei W, Zhang YJ, Chen MS, Guo RP, Li QJ, Shi M. Lenvatinib, toripalimab, plus hepatic arterial infusion chemotherapy versus lenvatinib alone for advanced hepatocellular carcinoma. Ther Adv Med Oncol. 2021 Mar 25;13:17588359211002720. doi: 10.1177/17588359211002720. PMID: 33854567; PMCID: PMC8010824.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言







#研究发现#
73
#患者预后#
70
#细胞癌#
47
#Oncol#
50
#瑞普利单抗#
62
#肝细胞#
45
#晚期肝细胞癌#
61
#回顾性研究#
58
#Med#
55