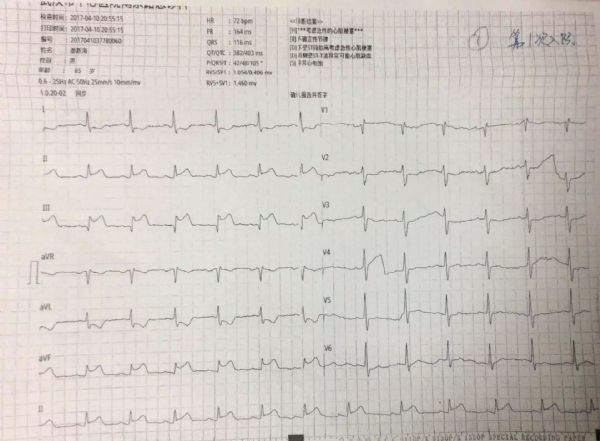
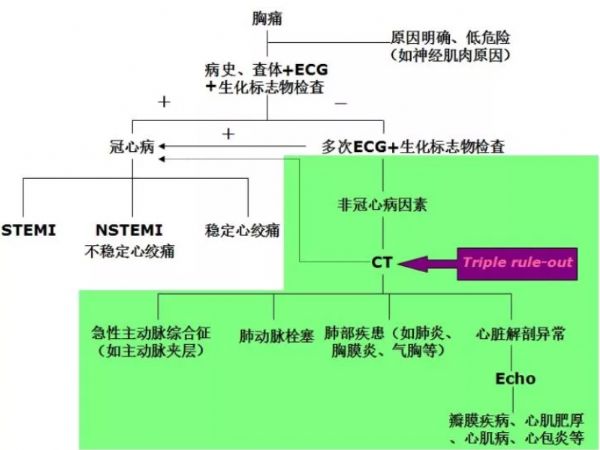
PCI术后呼吸困难,再梗?心衰?肺栓塞?药物?
2017-11-15 齐海军 (武汉市中心医院) MedSci原创
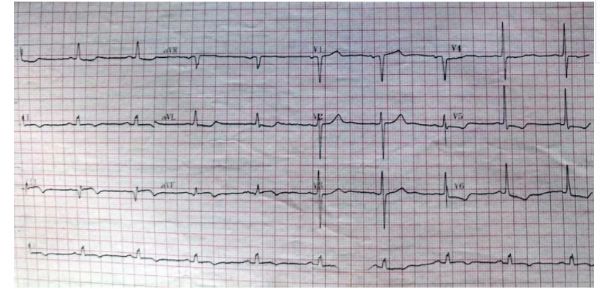
患者入院前3周因急性心梗入院,行右冠PCI术,近1周再次出现胸闷、气促。是何原因?如何完善辅助检查?如何调整用药?
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#PCI术#
53
#呼吸困难#
67
#PCI术后#
55
好
93
非常棒.认真学习
115
谢谢分享.阅读
74
好好好好好好好好就
66
学习了.谢谢分享
88