双靶标CAR-T细胞——实体肿瘤的克星
2018-08-12 悠然 生物探索
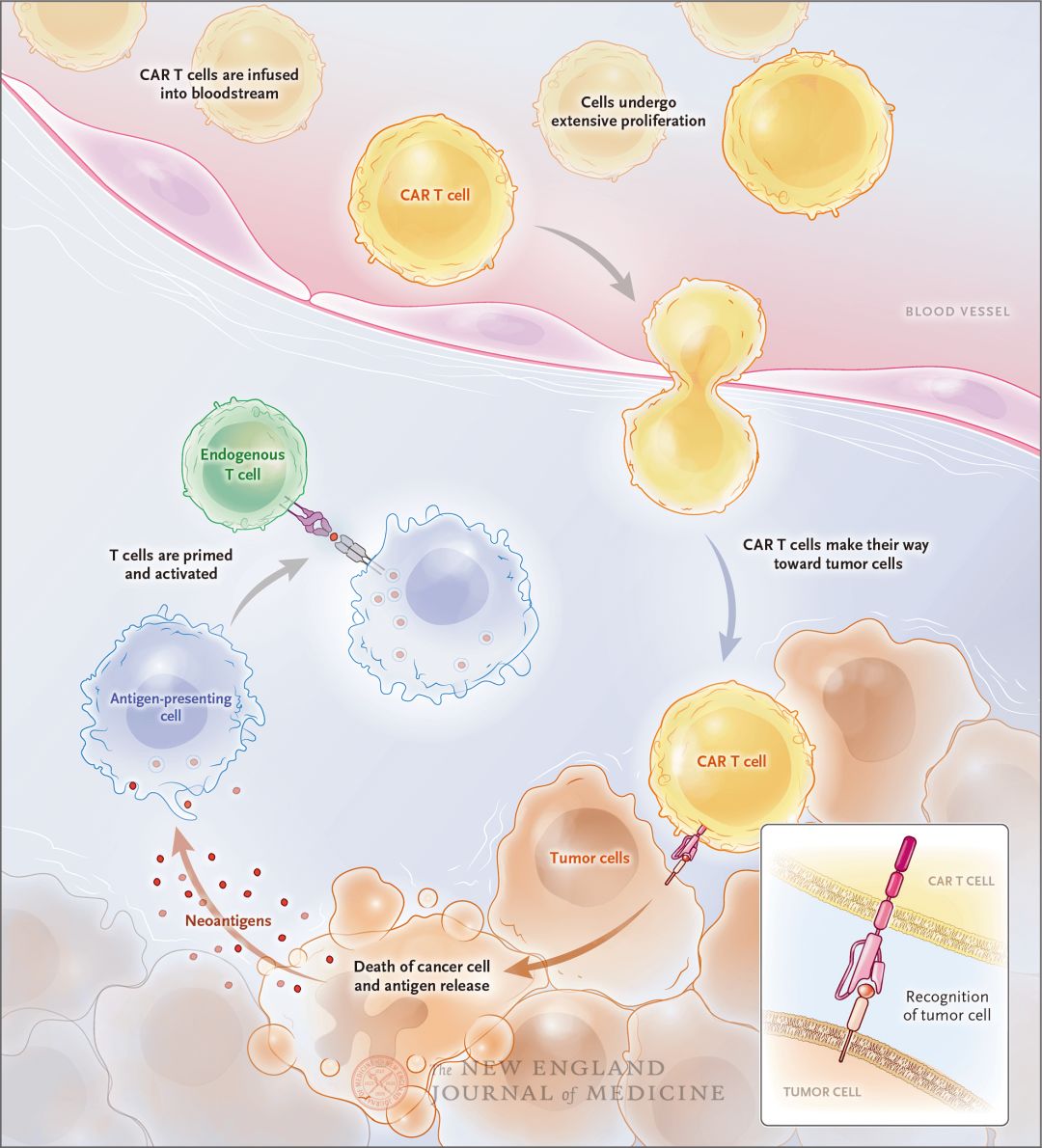
西雅图儿童医院最近开展了一项名为STRIvE-01的嵌合抗原受体(CAR-T)细胞免疫治疗试验,该试验适用于伴有EGFR蛋白表达的实体瘤儿童和青少年患者。在第1阶段试验中,双靶标的CAR-T细胞将更好地靶向儿童肉瘤、肾肿瘤和神经母细胞瘤等实体肿瘤中的EGFR蛋白。
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言











a:¥CnTwb1llNAq¥
71
#CAR-#
41
学习学习谢谢
64
#靶标#
45
#实体肿瘤#
47
学习
73