BMJ:高血压、吸烟、肥胖对中青年人的心衰发病影响,甚于高龄老年人
2021-07-26 心血管健康联盟 心血管健康联盟
心力衰竭是65岁以上老年人群住院的重要原因之一,临床上也将其认定为衰老相关的一类疾病。不过,过去十余年里,在青年、中年人群中,心衰发病例数越来越多,有必要对相关危险因素做进一步探明。
心力衰竭是65岁以上老年人群住院的重要原因之一,临床上也将其认定为衰老相关的一类疾病。不过,过去十余年里,在青年、中年人群中,心衰发病例数越来越多,有必要对相关危险因素做进一步探明。
美国麻省总医院学者评估了一般人群心衰危险因素的年龄差异,结果已发表在了四大医学杂志之一的《BMJ》上。
研究人员从弗雷明汉心脏研究 (FHS)、预防肾脏和血管终末期疾病研究(PREVEND)、动脉粥样硬化多种族研究 (MESA)三项大型流行病学队列研究中,共纳入24675例无心衰史参与者。依据年龄,分为青年(<55岁)、中年(55-64岁)、老年(65-74岁)、高龄(>75岁)四组。

图1:各年龄层人群的基线资料和临床数据
研究的中位随访时间长达12.7年,共统计到1381例心衰事件。四组人群(年龄由低到高)的心衰发病率分别为1%、5%、10%、18%,青年组、高龄组的中位心衰发病年龄分别为58岁、89岁。
其中,青年组的射血分数保留型/降低型心衰占比分别为32%、66%,高龄组为43%、41%。
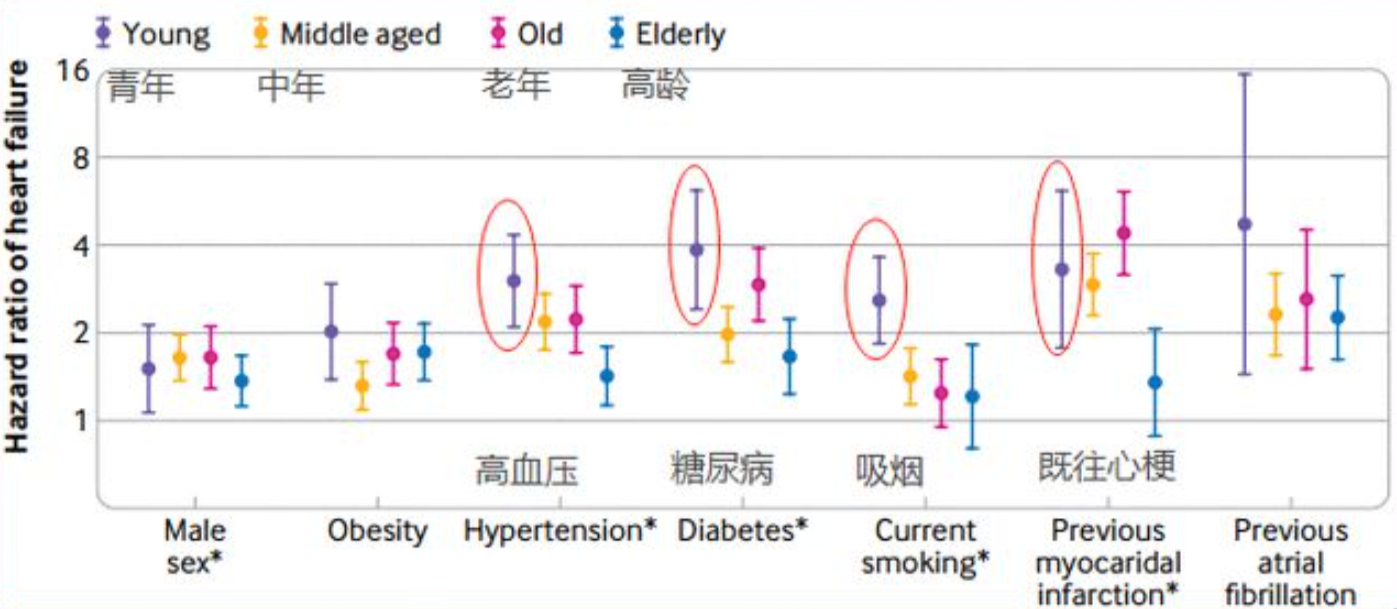
图:2:不同年龄层的各危险因素与心衰事件关联的森林图
同较年长人群相比,吸烟、高血压、糖尿病、既往心梗史,带给较年轻人群的心衰发病风险明显更高:
高血压可使青年组人群的心衰风险增加至原来的3倍,而仅使得高龄人群的心衰风险增加43%;
糖尿病可使青年、高龄人群的心衰风险风别增加至原来的3.86、1.66倍;
吸烟2.58、1.21倍,既往心梗史3.3、1.35倍。
无论有无危险因素,较年轻者发生心衰的绝对风险,均低于较年长者。
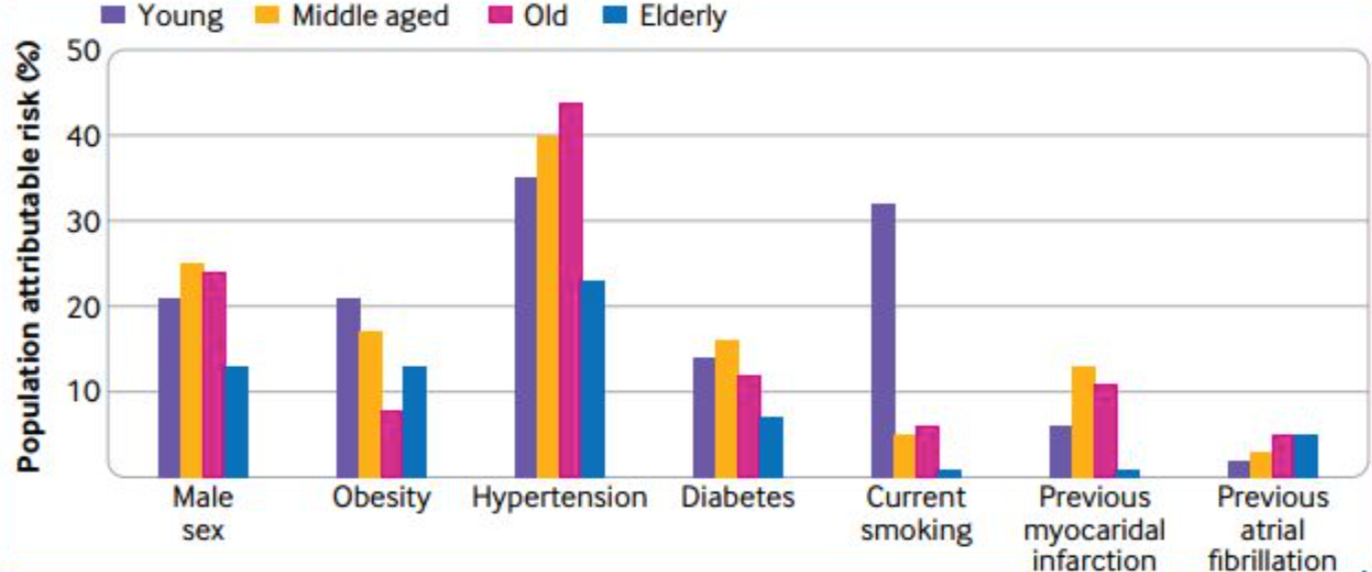
图3:不同年龄层发生心衰的各危险因素归因危险度柱状图
此外,除既往房颤史外,其他统计在内的各危险因素上,青年组对比高龄人群(75岁以上)的归因危险度均更高:
男性(21% v 13%),肥胖(21% v 13%),高血压 (35% v 23%),糖尿病(14% v 7%),吸烟(32% v 1%),既往心梗(6% v 1%)。
总的来说,虽然年轻人群的心衰发病率和绝对风险相对更低,但吸烟、高血压等危险因素对其的影响也更大,施以预防性措施调节可控因素,一定程度上可有效延缓或避免心衰的发生。
原始出处:
Jasper Tromp, et al. Age dependent associations of risk factors with heart failure: pooled population based cohort study. BMJ 2021; 372.
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#青年人#
60
#BMJ#
51
#高龄老年#
49
#高龄#
77
#中青年#
59
刚好需要这样的数据做比较
70
多运动,少吸烟
66
#学习#正好需要这个数据参考一下
71