NEJM:遗传性出血性毛细血管扩张-病例报道
2019-12-26 xing.T MedSci原创
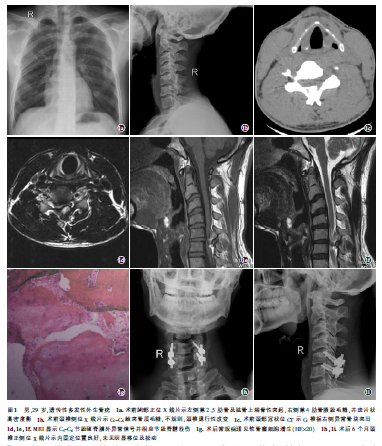
遗传性出血性毛细血管扩张(或Rendu–Osler–Weber综合征)是一种常染色体显性遗传疾病,导致血管畸形。在以下任何三种情况下进行临床诊断:复发性鼻出血、粘膜皮肤毛细血管扩张、内脏动静脉病变或有遗传性出血性毛细血管扩张的一级亲属。肺动静脉畸形可因栓塞导致卒中。

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言








#遗传性#
49
#毛细血管#
66
#血管扩张#
66
#扩张#
64
#毛细血管扩张#
58
顶刊就是顶刊,谢谢williamhill asia 带来这么高水平的研究报道,williamhill asia 科里同事经常看williamhill asia ,分享williamhill asia 上的信息
66