durvalumab联合tremelimumab治疗膀胱癌:无法改善OS
2020-03-08 Allan MedSci原创
阿斯利康近日宣布,一项针对PD-L1抑制剂Imfinzi(durvalumab)的III期研究(单药治疗以及与抗CTLA4抗体tremelimumab联合使用)未能达到主要终点。
阿斯利康近日宣布,一项针对PD-L1抑制剂Imfinzi(durvalumab)的III期研究(单药治疗以及与抗CTLA4抗体tremelimumab联合使用)未能达到主要终点,该项临床试验的主要终点为Imfinzi(durvalumab)治疗无法切除的IV期膀胱癌患者的总体生存(OS)。
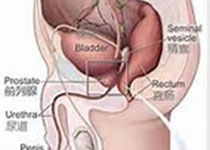
在DANUBE试验中,对于肿瘤细胞和/或浸润肿瘤的免疫细胞表达高水平PD-L1的患者,Imfinzi单一疗法不能改善患者的OS,Imfinzi和tremelimumab的组合也不能改善OS,且不论患者肿瘤细胞PD-L1表达水平如何。阿斯利康肿瘤学研发执行副总裁José Baselga表示:“这些结果将为williamhill asia 全面的膀胱癌III期开发计划提供参考”。膀胱癌泛指各种出自膀胱的恶性肿瘤,也就是有异常细胞大量增殖而不受管制。膀胱是贮存尿液的中空器官,外壁主要由肌肉构成,位于下腹部。最常见的膀胱癌细胞来自膀胱内面黏膜表皮,正式名称为移行上皮细胞癌(TCC)。
原始出处:
https://www.firstwordpharma.com/node/1706245
本文系williamhill asia 医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言


















#TREM#
67
#mAb#
43
#REM#
41
#Tremelimumab#
63
膀胱癌真怪,明明是免疫敏感性肿瘤,为什么PD-1治疗效果不好呢?难道靶点不对?将来CD47会不会有效
58