Int J Cardiol:急性冠状动脉综合征患者卒中的发生率和预测因素
2018-11-05 xing.T MedSci原创
由此可见,ACS后卒中的长期发生率为3.8%,AF患者为7.8%,无AF的患者为3.3%。
卒中是最令人恐惧的心血管疾病之一,因为它具有高度的致残风险,并且其在急性冠状动脉综合征(ACS)后的发病率并不少见。
近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,研究人员对在两家医院连续就诊的所有ACS患者进行了回顾性研究。将全因死亡率作为竞争事件的竞争风险回归用于评估卒中发病率。
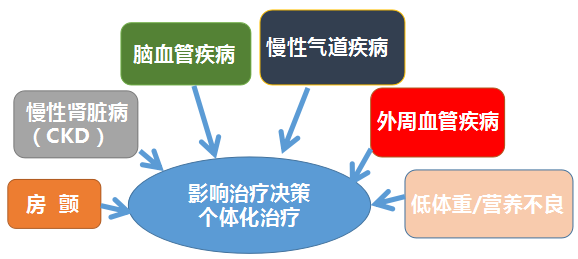
研究人员纳入了8771例患者,房颤患病率为12.4%。AF患者年龄较大,心血管危险因素和既往心血管疾病患病率越高,并且肾小球滤过率较低。不到一半的AF患者在入院前接受口服抗凝治疗。院内死亡率为5.1%,AF患者的死亡率高出两倍多(10.2% vs. 4.4%; p<0.01)。在出院时观察到医学治疗的相关差异,并且在AF患者中口服抗凝剂的比例大约<50%。中位随访期间为58.7个月,313例患者至少发生一次卒中(发生率为3.8%,95%CI为3.4-4.2),AF患者高出2倍:7.8% vs. 3.3%(p<0.01)。首次卒中的中位时间为33.0(30.1)个月,AF患者与非AF患者相比时间更短(28.2±22.3 vs. 34.6±31.1; p<0.01)。调整后的竞争风险回归确定了AF、既往卒中和CHA2DS2-VASc评分=2或≥3作为卒中的独立预测因子; CHA2DS2-VASc评分=2仅与AF患者的卒中风险相关。
由此可见,ACS后卒中的长期发生率为3.8%,AF患者为7.8%,无AF的患者为3.3%。
原始出处:
AlbertoCordero,et al.Incidence and predictors of stroke in patients discharged with the diagnosis of acute coronary syndrome.International Journal of Cardiology.2018.https://doi.org/10.1016/j.ijcard.2018.10.082
本文系williamhill asia
医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#发生率#
41
#Cardiol#
50
#冠状动脉综合征#
41
房颤流行病学
79
#预测因素#
53
#综合征#
37
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
57