Cardiovasc Diabetol:糖尿病肾病患者中SGLT2抑制剂与心血管、肾脏和安全性结局的关系
2022-04-28 从医路漫漫 MedSci原创
钠-葡萄糖协同转运蛋白2抑制剂(SGLT2i)最近成为一种新型口服降糖药物,具有多效作用,包括减少T2D患者的心血管和肾脏预后。
背景:2型糖尿病(T2D)在美国仍然非常普遍。目前有近3200万美国人感染了T2D病毒,预计其患病率将会上升。糖尿病相关的微血管并发症如糖尿病肾病(DKD)构成了一个重大的公共卫生问题。事实上,近40%的T2D患者发展为DKD。DKD是慢性肾病(CKD)和终末期肾病(ESKD)的主要原因。此外,在糖尿病患者中观察到的大多数额外死亡风险可能与DKD的存在有关。钠-葡萄糖协同转运蛋白2抑制剂(SGLT2i)最近成为一种新型口服降糖药物,具有多效作用,包括减少T2D患者的心血管和肾脏预后。DKD患者的SGLT2i处方稳步增加。然而,SGLT2i对DKD全境的影响仍存在一些不确定性。例如,在SGLT2i的早期临床试验中,相对较少的参与者达到了ESKD。关于SGLT2i对DKD患者中风等临床结果影响的研究得出了不一致的结果。此外,针对SGLT2i的心血管结局试验通常不足以评估DKD患者的大多数不良事件。
目的:williamhill asia 对主要的心血管和肾脏结局试验进行了系统回顾和荟萃分析,以总结和更新目前可用的关于SGLT2i对DKD患者心血管、肾脏和安全性结局影响的证据。
方法:williamhill asia 在电子数据库中搜索截至2021年9月30日发表的主要随机安慰剂对照临床试验,并报道SGLT2i治疗DKD患者的心血管和肾脏结果。DKD被定义为二型糖尿病患者的慢性肾脏疾病。随机效应荟萃分析模型用于评估临床结果的合并风险比(HR)和95%可信区间(CI),包括主要不良心血管事件(MACE:心肌梗死[MI]、中风和心血管死亡)、肾脏综合结果(肾功能恶化、终末期肾病或肾脏或心血管原因死亡的组合)、心力衰竭住院(HHF)、死亡和安全事件(霉菌感染、糖尿病酮症酸中毒[DKA]、容量衰竭、截肢、骨折、尿路感染[UTI]、急性肾损伤[AKI]和高钾血症)。
结果:来自8个大规模试验的26,106名DKD患者被纳入研究(中位年龄:65.2岁,29.7-41.8%为女性,53.2-93.2%为白人,中位随访时间:2.5年)。SGLT2i与MACE (HR 0.83,95% CI 0.75–0.93)、肾脏综合结果(HR 0.66,95% CI 0.58–0.75)、HHF (HR 0.62,95% CI 0.55–0.71)、心血管死亡(HR 0.84,95% CI 0.74–0.96)、心肌梗死(HR 0.78,95% CI 0.67–0.92)、中风(HR在估计肾小球滤过率降低(eGFR: < 60 mL/min/1.73m2)的参与者中观察到类似的结果。男性和女性发生真菌感染的相对风险(95% CI)分别为3.89(1.42–10.62)和2.50(1.32–4.72),DKA为3.54(0.82–15.39),容量衰竭为1.29(1.13–1.48)。
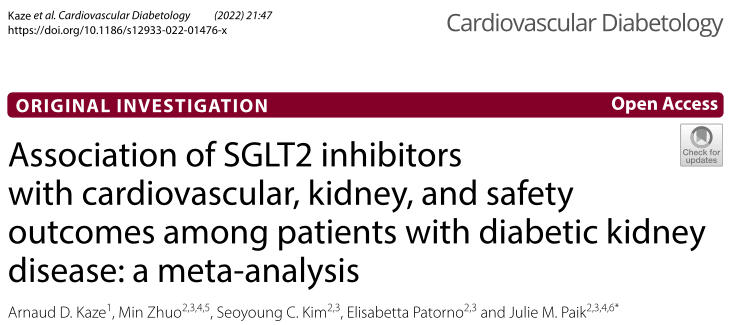
表1 SGLT-2抑制剂对成人糖尿病肾病临床结果的影响
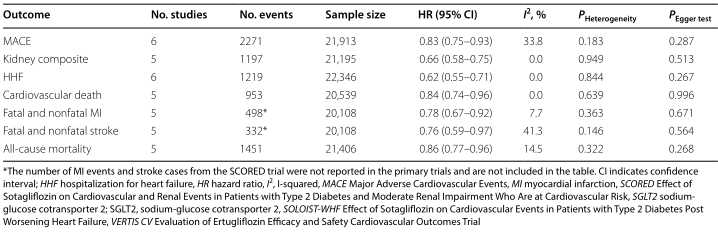
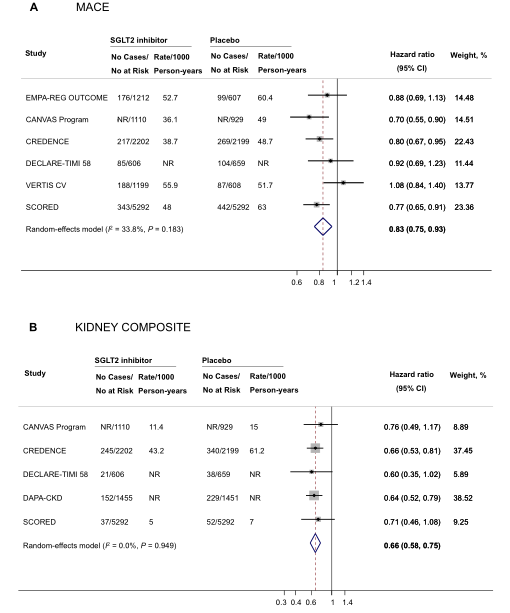
图1 SGLT22抑制剂对糖尿病肾病患者主要心血管不良事件(A)和肾脏综合结果(B)的影响。
表2 SGLT22抑制剂对eGFR降低参与者临床结果的影响
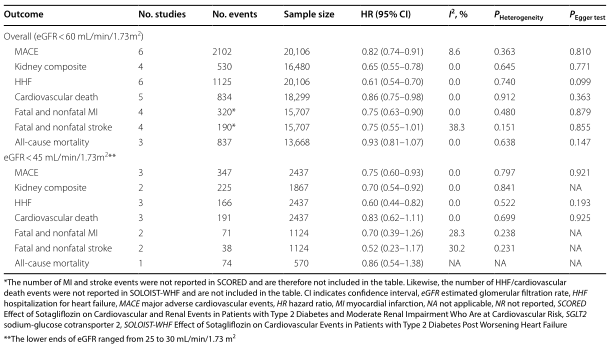
表3 SGLT2抑制剂对中度或重度蛋白尿患者临床结果的影响

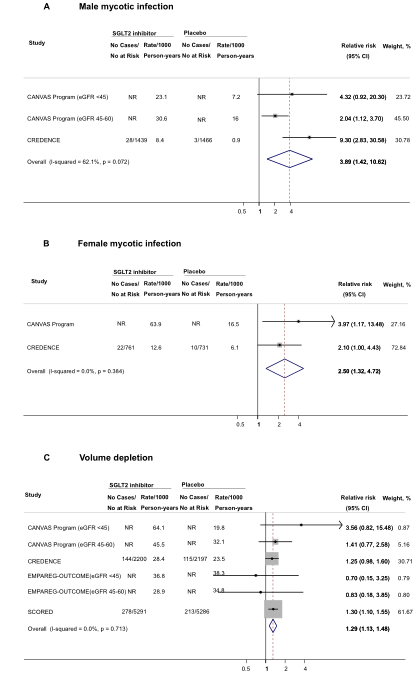
图2 SGLT2抑制剂对糖尿病肾病患者安全性结果的影响。
结论:在患有DKD的成年人中,SGLT2i与MACE、肾脏转归、HHF和死亡的风险降低相关。除了更明确的安全信号的少数例外,williamhill asia 发现SGLT2i和安全结果之间的联系的总体数据有限。需要对SGLT2i在该人群中的安全性进行更多的研究。
原文出处: Kaze AD, Zhuo M, Kim SC,et al.Association of SGLT2 inhibitors with cardiovascular, kidney, and safety outcomes among patients with diabetic kidney disease: a meta-analysis.Cardiovasc Diabetol 2022 Mar 23;21(1)
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言













#BET#
58
#2抑制剂#
47
#ASC#
55
#DIA#
54
#肾病患者#
0
#抑制剂#
0
#SGLT#
57
***,
64
#SGLT2#
57