Dig Liver Dis:小儿炎症性肠病患者使用免疫调节剂的长期结果
2020-03-14 MedSci原创 MedSci原创
在新的生物制剂越来越获得认可的时代,williamhill asia 需要重新评估免疫调节剂在小儿炎症性肠病(IBD)治疗中的地位。
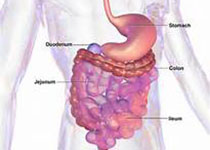
背景及目标:在新的生物制剂越来越获得认可的时代,williamhill asia 需要重新评估免疫调节剂在小儿炎症性肠病(IBD)治疗中的地位。
方法:研究人员回顾了过去10年来所有克罗恩病(CD)或溃疡性结肠炎(UC)儿童的临床数据,将自诊断以来接受常规治疗的儿童(包括5-氨基水杨酸酯,类固醇,硫嘌呤和甲氨蝶呤)包括在内。主要结果是在诊断后6个月和12个月以及最后的随访中无类固醇的临床缓解,无需抢救治疗(生物制剂或手术)。进行Cox比例风险建模以确定与结果相关的诊断变量。
结果:总共纳入176名IBD患者(121 CD,55 UC),中位随访时间为4.6 [2.0-8.1]年。第6个月的缓解率是79.6%,但在第12个月时降低到60.2%,在最后的随访中降低到31.8%。CD患者的CRP较高[1.006(1.001-1.011)],白蛋白较低[1.050(1.012–1.086)]和生长障碍[1.214(1.014–1.373)],PUCAI评分较高[1.038(1.006-1.072)]和低铁UC患者的[1.023(1.003-1.043)]与治疗失败相关(p <0.05)。
结论:诊断后5年,只有32%的小儿IBD患者将保持无生物制剂或手术治疗。
原始出处:
Karen van Hoeve. Et al.Long-term outcome of immunomodulator use in pediatric patients with inflammatory bowel disease. Digestive and Liver Disease. 2020
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#长期结果#
59
#Dis#
60
#炎症性#
73
#炎症性肠病患者#
60
文编刊医论
137