Blood:JAK2 V617F和CALR突变的人群发生率和表现
2019-06-24 MedSci MedSci原创
JAK2 V617F和calrenetin突变(CALR)是骨髓增生性肿瘤(MPN)中常见的驱动突变。在普通人群中可检测到JAK2 V617F,但尚无研究调查CALR的发生率。Sabrina Cordua等人开展研究来明确CALR和JAK2 V617F的人群发生率,同时评估有携带这两个突变的MPN患者和非MPN患者的生化特征和生活方式风险因素。2010年-2013年,共招募了19 958位受试者,
Sabrina Cordua等人开展研究来明确CALR和JAK2 V617F的人群发生率,同时评估有携带这两个突变的MPN患者和非MPN患者的生化特征和生活方式风险因素。
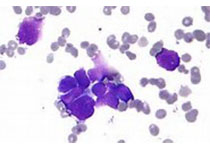
2010年-2013年,共招募了19 958位受试者,通过数字PCR来筛查JAK2 V617F和CALR。645位受试者携带阳性突变(3.5%),其中16位(2.5%)在起始时即患有MPN。613位受试者为JAK2 V617F阳性(等位基因负荷[平均{SE}:2.1{0.34}%),32位受试者为CALR阳性(等位基因负荷:7.5{2.2}%),与人群发生率相符(分别为3.1%[CI 2.8-3.3%]和0.16%[CI 0.11-0.23%])。年龄增长、吸烟和酒精均是突变的危险因素。
突变阳性的血细胞计数高于无突变的血细胞计数,40%的阳性突变的非MPN患者的血细胞计数高于或等于对照的。
总而言之,本研究展现了新的CALR和JAK2 V617F的人群发生率,要比敏感性差的方法高出3-30倍。突变阳性的非MPNs患者的血细胞计数增多,有助于引起对人群中MPN诊断不足的关注。
Sabrina Cordua, et al.Prevalence and phenotypes of JAK2 V617F and Calreticulin mutations in a Danish general population. Blood 2019 :blood.2019001113; doi: https://doi.org/10.1182/blood.2019001113
本文系williamhill asia 医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言










#JAK#
112
#CALR突变#
81
#CALR#
100
#发生率#
58
#JAK2#
97