Theranostics:北大张韬团队从单细胞角度揭秘主动脉夹层发病机制
2022-03-27 科学前沿 科学前沿
该研究既证明了单细胞测序技术在临床诊断方面的作用,也为日后AD的早期预诊和快速分诊提供了可能。
近日,主动脉夹层(AD)发病机制又有了新发现。北京大学人民医院血管外科张韬课题组联合中国医学科学院阜外医院心血管疾病国家重点实验室王利教授课题组和解放军总医院第一医学中心、全军血管外科中心郭伟教授课题组在Theranostics杂志(IF 11.556)上发表了题为“Dysregulation of interaction between LOXhigh fibroblast and smooth muscle cells contributes to the pathogenesis of aortic dissection”(成纤维细胞与平滑肌细胞之间相互作用的失调是主动脉夹层的发病机制之一)的相关研究。该研究找到药物治疗AD的新靶点,并为实现AD早期预诊和快速分诊提供了可能。
Theranostics期刊发表的创新研究文章主要关注于体外诊断和预后、体内分子成像、分子治疗、图像引导治疗、生物传感器、系统生物学和转化医学、个性化医学和广泛的生物医学研究领域,可应用于未来的治疗诊断应用。

主动脉夹层(AD),可发生于任何年龄,是临床常见、最复杂最危险的主动脉疾患之一。一旦破裂出血,患者未能及时诊治,病死率极高。
主动脉是最大的动脉血管,分为外膜、中膜和内膜三层,其中外膜主要由包绕的结缔组织、分布的神经末梢、弹力膜等构成,中膜主要由平滑肌细胞及细胞外基质构成,内膜主要由内皮细胞构成。AD,主要是主动脉腔内的血流从内膜撕裂口进入中膜,在血管壁分裂成真、假腔而形成。国际急性主动脉夹层注册(IRAD)数据显示,AD最常见的诱发因素是高血压和动脉粥样硬化。
据研究表明,AD发病基础主要在中膜结构发生异常,也就是平滑肌细胞发生退变。而外膜的成纤维细胞被认为是为中膜提供营养物质。但如果主动脉血管出现损伤后,炎症反应会最早出现在外膜,又因多重因素而改变血管结构及功能的完整性,而导致夹层的发生。
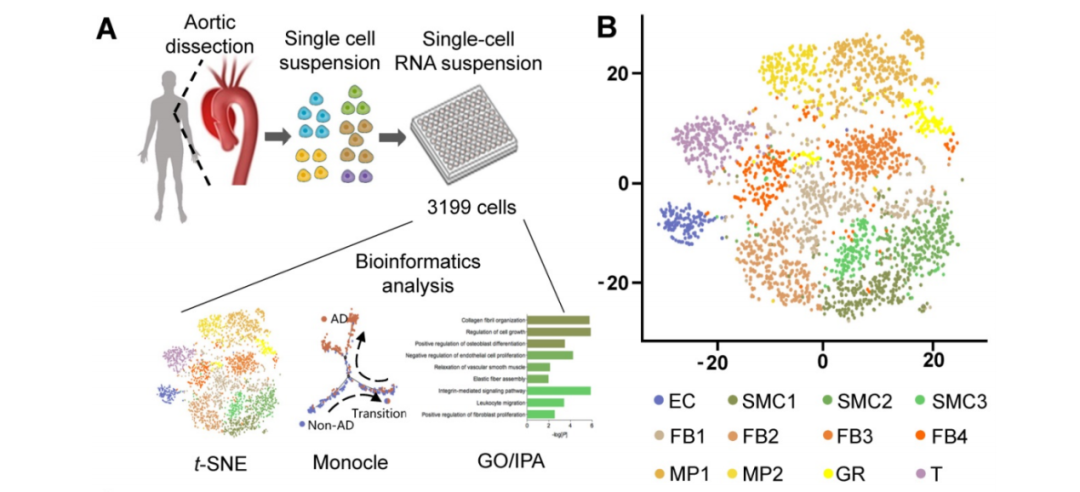
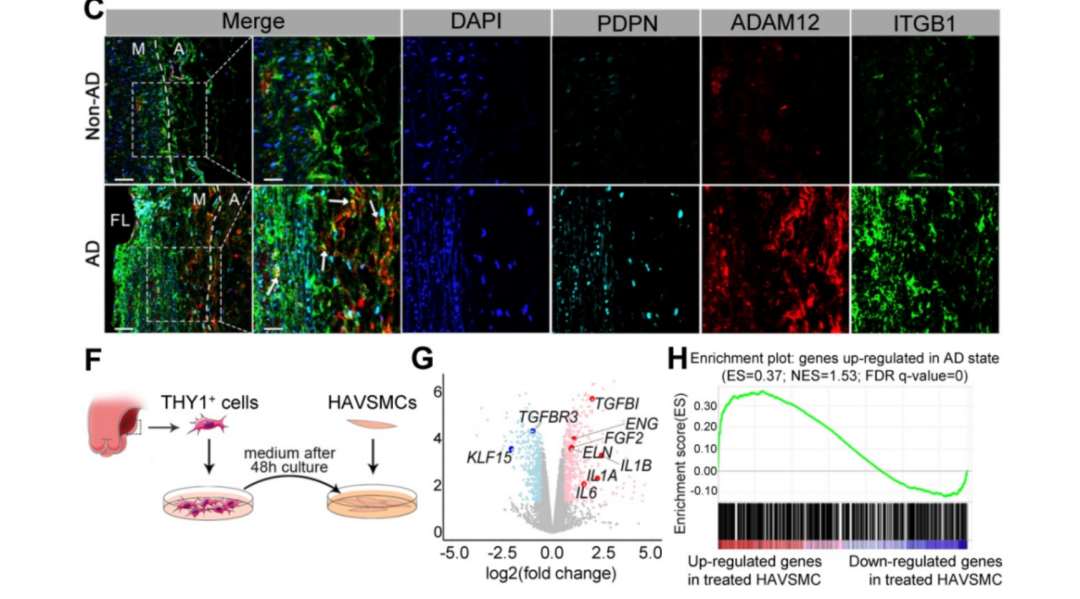
张韬课题组专注于探索血管稳态和疾病发展中细胞间的相互作用和功能靶点。该课题通过单细胞转录组测序和免疫多色染色技术,首次描述了正常人胸主动脉和Stanford A型AD患者病变血管中细胞亚群组成及其空间位置,同时研究发现AD标本中高表达的LOX成纤维细胞亚群(FB2)表达谱会随着AD病理发展进程显著变化;导致其与血管平滑肌细胞(VSMC)的异常细胞亚群产生相互作用,共同促进AD发展。通过抑制小鼠血管外膜中的BMP(骨形态发生蛋白)信号通路可以有效抑制FB2的状态转化,进而降低小鼠AD的发生率。
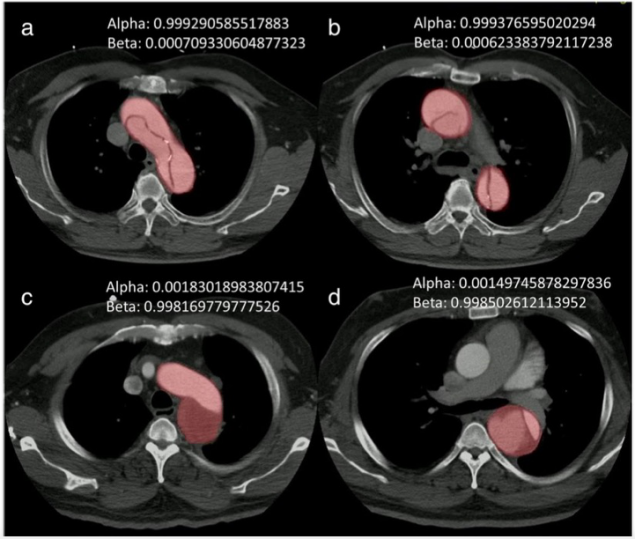
从临床角度而言,基于前期单细胞数据,课题组筛选出了FB2特异性分泌蛋白COL5A1,并验证其在AD患者血浆中的浓度显著高于对照组,首次阐述其作为AD血液生物标志物的可能性。简而言之,通过单细胞测序技术,不仅确定了特定FB细胞亚群在AD发生发展中的关键作用,还揭示了细胞间相互作用的动态变化及其在血管疾病病理生理过程中的重要作用。
该项研究证明了从调控细胞间相互作用的角度治疗AD的可行性,既为以后AD的治疗提供了新思路,也为日后AD的药物治疗找到了新的靶点,即抑制成纤维细胞的状态转化。同时,这项研究首次通过单细胞测序技术完成了AD生物标志物的筛选,既证明了单细胞测序技术在临床诊断方面的作用,也为日后AD的早期预诊和快速分诊提供了可能。
部分研究数据和图示
该项研究受到国家自然科学基金及国家重点研发计划项目基金项目的支持。张韬、陈奕男和姚芳是该论文的并列第一作者。王利、郭伟和周冰莹为共同通信作者。
原始出处
Dysregulation of interaction between LOXhigh fibroblast and smooth muscle cells contributes to the pathogenesis of aortic dissection.Theranostics.2022
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#Theranos#
72
#ERA#
72
不错
68
又有新收获。
64
#主动脉#
0
#动脉夹层#
61