J INTERN MED:噬血细胞性淋巴组织细胞增生症的发病率和存活率
2021-12-08 MedSci原创 MedSci原创
英格兰噬血细胞性淋巴组织细胞增生症的诊断在2000年至2016年期间有所增加。75岁以上和血液系统恶性肿瘤患者的一年生存率差异很大。
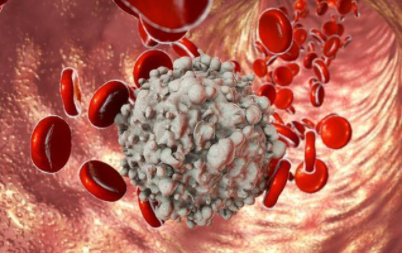
噬血细胞性淋巴组织细胞增生症是一种罕见的高炎症性疾病,患者预后不佳。很少有基于人群的成人发病率和存活率估计值。
近日,内科学领域权威杂志Journal of Internal Medicine上发表一篇研究文章,研究人员旨在在英格兰进行这项研究,以提供这些数据。
研究人员使用来自英格兰初级保健、二级保健、癌症登记和死亡率数据库的基于人群的关联数据来确定2000年1月1日至2016年12月31日期间诊断为噬血细胞性淋巴组织细胞增生症的个体。研究人员按年龄和性别计算了噬血细胞性淋巴组织细胞增生症的年发病率,并使用泊松回归模拟发病率随时间的变化。此外,研究人员使用Kaplan-Meier方法计算了受试者的总体1年生存率,并使用Cox比例风险模型估计调整后的死亡风险比(HR)。
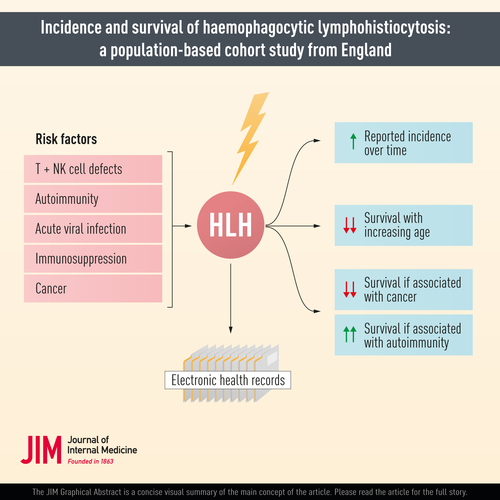
研究人员确定了214名噬血细胞性淋巴组织细胞增生症患者。该研究报告的年龄和性别调整后的发病率在此期间增加了2倍,从百万分之一增加到约百万分之二。1岁以下(每百万人14.6人)和75岁以上(每百万人2.2人)的个体发病率最高,15-44岁的个体发病率最低(每百万人0.8人)。一年生存率因年龄和性别而异,从15岁以下的77%(95%CI为63%至86%)到75岁以上的30%(95%CI为14%至49%)不等。在血液系统癌症患者中,与没有恶性疾病或风湿病疾病的患者相比,调整后的死亡HR为2.60(95%CI为1.45至4.66)。
由此可见,英格兰噬血细胞性淋巴组织细胞增生症的诊断在2000年至2016年期间有所增加。75岁以上和血液系统恶性肿瘤患者的一年生存率差异很大。
原始出处:
Joe West,et al.Incidence and survival of haemophagocytic lymphohistiocytosis: A population-based cohort study from England.Journal of Internal Medicine.2021.https://onlinelibrary.wiley.com/doi/10.1111/joim.13432
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言









#存活率#
67
#发病率#
60
#血细胞#
60
#细胞性#
71
#Med#
55
有用,学习了
92