经皮脊柱内镜处理双节段腰椎管狭窄症合并椎管内骨化三例
2019-02-25 周庆 孔清泉 张斌 中国骨与关节杂志
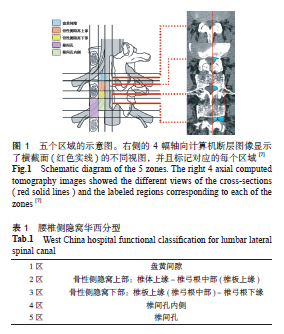
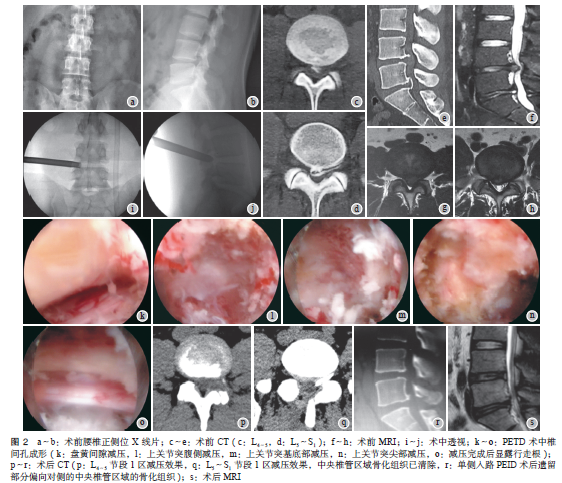
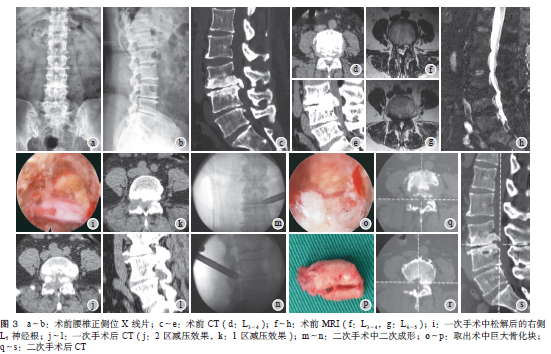
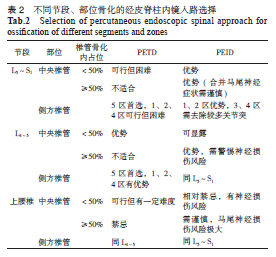
腰椎管狭窄症(LSS)包括发育性椎管狭窄和继发性椎管狭窄,继发性椎管狭窄原因包括退变性椎管狭窄、椎管内骨化所导致的狭窄、肿瘤性狭窄和外伤性狭窄等。骨化性疾病导致的继发性LSS包括椎体后缘离断(PRAS),后纵韧带、纤维环、黄韧带的骨化或钙化等。目前经皮脊柱内镜技术(PED)已逐渐成为治疗LSS的主要手术方式之一。文献报道经皮内镜下腰椎椎管减压术(PELD)治疗合并同节段PRAS、后纵韧带骨化和纤维

本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言












#椎管#
58
#椎管内#
60
#椎管狭窄#
63
#内镜#
52
#腰椎#
53
#腰椎管狭窄症#
78
#腰椎管狭窄#
53
#腰椎管#
42