Nature Communication:靶向转录因子JunB抑制致病性TH17细胞导致的自免疫疾病
2017-06-01 MedSci MedSci原创
这一研究证明了JunB是依赖IL-23所分化的致病性TH17细胞的重要决定因素,有潜力成为治疗因致病性TH17细胞失衡产生的自身免疫性疾病的治疗靶点。
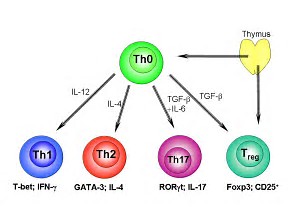
在各种CD4+的T辅助(T helper)细胞中,能够分泌细胞激素IL17的细胞被称为TH17细胞。早期研究对于其在机体和疾病模型中的表现,意见不一。一方面认为其为促进炎症导致疾病的细胞,另一方面认为其不具有明显的促炎功能。随着研究的进行,尽管TH17细胞共同的被RORγt转录因子控制调控其分化,但是根据其所分泌的细胞因子不同,TH17细胞被进一步归类为受TGFbeta和IL6所刺激分化的非致病性TH17(non-pathogenic T cell),和受IL6,IL1beta,IL23所刺激诱导分化的致病性TH17细胞。
通过移植这两种不同的TH17细胞到免疫缺陷的老鼠体内,致病性TH17细胞会引起强烈的免疫反应,包括肠炎和多发性硬化症,而非致病性TH17细胞则不会引起这类疾病。这两类细胞在各自的基因调控过程中,到底有什么不同并不是很清楚。
在最新的一期Nature Communication杂志中,Zafrul Hasan及其同事报道了他们的发现,属于AP-1转录因子的JunB蛋白在致病性TH17细胞中有更高的表达,并且对于其致病性至关重要。在致病性TH17细胞中,细胞因子IL-6会诱导JunB蛋白的表达,从而促进下游的转录因子BATF结合DNA,帮助对于致病性TH17细胞分化起到重要作用的RORγt和IL23受体的表达。但是,这一信号通路在受TGFβ1刺激所产生的非致病TH17细胞中则不存在。
通过基因编辑,研究人员证明在缺乏Junb基因的T细胞中,不能被诱导成为致病性TH17细胞。而移植缺乏JunB基因的T细胞到实验小鼠中,则不能产生自身免疫性脑脊髓炎和结肠炎。然而,JunB缺乏症并不影响肠道非致病性TH17细胞的数量。
这一研究证明了JunB是依赖IL-23所分化的致病性TH17细胞的重要决定因素,有潜力成为治疗因致病性TH17细胞失衡产生的自身免疫性疾病的治疗靶点。
原始出处:
Zafrul Hasan et al., JunB is essential for IL-23-dependent pathogenicity of Th17 cells. Nature Communications 8, Article number: 15628 (2017)doi:10.1038/ncomms15628
本文系williamhill asia
医学(MedSci)原创编译整理,转载需授权!
小提示:本篇威廉亚洲官网
需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言
本网站所有内容来源注明为“williamhill asia 医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于williamhill asia 医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“williamhill asia 医学”。其它来源的文章系转载文章,或“williamhill asia 号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与williamhill asia 联系,williamhill asia 将立即进行删除处理。
在此留言







#转录#
50
#Nat#
50
#COMMUN#
46
#致病性#
57
#Th17#
49
#免疫疾病#
35
#转录因子#
42